The recently emergent field of Nanotechnology involves the production and use of structures at the nanoscale. Research at atomic, molecular or macromolecular levels, has led to new materials, systems and structures on a scale consisting of particles less than 100nm and showing unique and unusual physical, chemical and biological properties, which has enabled new applications in diverse fields, creating a multimillion-dollar high-tech industry. Nanotechnologies have a wide variety of uses from nanomedicine, consumer goods, electronics, communications and computing to environmental applications, efficient energy sources, agriculture, water purification, textiles, and aerospace industry, among many others.
The different characteristics of nanoparticles such as size, shape, surface charge, chemical properties, solubility and degree of agglomeration will determine their effects on biological systems and human health, and the likelihood of respiratory hazards. There are a number of new studies about the potential occupational and environmental effects of nanoparticles and general precautionary measures are now fully justified.
Adverse respiratory effects include multifocal granulomas, peribronchial inflammation, progressive interstitial fibrosis, chronic inflammatory responses, collagen deposition and oxidative stress.
The authors present an overview of the most important studies about respiratory nanotoxicology and the effects of nanoparticles and engineered nanomaterials on the respiratory system.
O campo recentemente emergente da nanotecnologia envolve a produção e o uso de estruturas em nanoescala. A pesquisa a níveis atómicos, moleculares e macro moleculares conduziu a novos materiais, sistemas e estruturas numa escala constituída por partículas menores que 100nm, apresentando propriedades físicas, químicas e biológicas únicas e incomuns, o que tem permitido novas aplicações em diversos campos, criando uma indústria de alta tecnologia multimilionária. As nanotecnologias têm uma vasta variedade de usos, desde a nano medicina, bens de consumo, eletrónica, comunicações e informática, até às aplicações ambientais, fontes de eficiência energética, agricultura, purificação de água, têxteis e indústria aeroespacial, entre muitos outros.
As diferentes características das nanopartículas, tais como tamanho, forma, carga de superfície, propriedades químicas, solubilidade e grau de aglomeração, determinarão os efeitos sobre os sistemas biológicos e na saúde humana e a probabilidade de riscos respiratórios. Existem alguns novos estudos sobre os potenciais efeitos ocupacionais e ambientais das nanopartículas, sendo totalmente justificadas as medidas gerais de precaução.
Os efeitos respiratórios adversos incluem granulomas multifocais, inflamação peribrônquica, fibrose intersticial progressiva, respostas inflamatórias crónicas, deposição de colagénio e stress oxidativo.
Os autores apresentam um resumo dos mais importantes estudos sobre nanotoxicologia respiratória e dos efeitos das nanopartículas e dos nanomateriais artificiais sobre o sistema respiratório.
The second half of the XX Century saw the emergence of a truly revolutionary era of nanotechnology.
The development of new materials, systems and structures through research at atomic, molecular, or macromolecular levels has enabled new applications.
The nanoscale is typically a scale of matter under 100nm. According to several authors, unique and unusual physical, chemical, and biological properties can be seen at this dimensional level.
Nanotechnology involves imaging, measuring, modeling, and manipulating matter at this scale. Some of the most promising uses of these technologies have emerged in some fundamental sectors, such as energy, communications, water purification, pollution reduction and environmental progress, improved materials and new products, medical and biomedical applications.1,2
Besides industrial and household uses, nanoparticles (NPs) can be used in Medicine (creating the new field of nanomedicine) for cancer treatment, infectious diseases, immunization purposes and diagnostic procedures with new imaging sensors and agents.3,4
As nanotechnology penetrates the marketplace and attracts attention, the public is starting to develop opinions about it. Those opinions will shape the market for consumer goods using these new technologies.5
Nanotechnology is a sector of high-tech industry that has already created a multibillion $US market, and is widely expected to grow to 1 trillion (1018) US dollars by 2015.6
Nanotechnology research and development can integrate the nanoscale structures into larger material components, systems, and architectures.7
The majority of the NPs currently in use today have been made from transition metals, silicon, different forms of carbon (carbon nanotubes; fullerenes), and metal oxides (such as zinc dioxide and titanium dioxide).
In sensu lato, inorganic nanoparticles do not contain carbon molecules; carbon nanotubes and carbon fullerenes are usually addressed as organic nanoparticles. But it must be stated that, strictly from a chemical point of view, these forms containing pure carbon molecules without bonds to hydrogen, constitute allotropes of carbon and are part of what is now known as the Inorganic Chemistry of Carbon.
New applications are constantly emerging. The Nanotechnology Consumer Products Inventory, kept by the Woodrow Wilson Institute, listed over 1317 products or product lines as of April 2012.8
Nanomaterials vary widely in terms of their composition, properties, and uses. Common products include cosmetics and personal care products, wound dressing pads, pregnancy tests, toothpaste, food supplements and food storage, appliances, clothing, coatings, electronics and computers and sporting goods.5
With the increasing technological complexity of nanotechnology, several generations of NPs can be reported:
First generation ∼2001: Passive nanostructures (nanostructured coatings, nanoparticles, nanostructured metals, polymers, ceramics, catalysts, composites, displays).
Second generation ∼2007: Active nanostructures (transistors, amplifiers, targeted drugs and chemicals, actuators, adaptive structures, sensors, diagnostic assays, fuel cells, solar cells, high performance nanocomposites, ceramics, metals).
Third generation ∼2010: 3-D nanosystems and systems of nanosystems (various assembly techniques, networking at the nanoscale and new architectures, biomimetic materials, novel therapeutics/targeted drug delivery).
Fourth generation ∼2015: Molecular nanosystems (molecular devices “by design”, atomic design, emerging functions).9
The expression “nanoparticle” is commonly used to describe engineered structures with diameters of <100nm, that are created by chemical and/or physical processes, with very characteristic properties usually not present at a macro-scale level.10
Reducing the size of a particle increases the ratio of surface area to mass. Because the reactive portion of the particle is on the surface, increasing the relative surface area will increase reactivity of a given amount of material. Also, at the nanoscale, both classical physics and quantum physics can direct the behaviour of a particle. The influence of quantum effects can change important material properties, such as optical, magnetic, and electrical properties.5
NPs may be suspended in a gas (as a nanoaerosol), suspended in a liquid (as a colloid or nano-hydrosol), or embedded in a matrix (as a nanocomposite).11
Some authors state that the main difference between NPs and ultrafine particles (UFP) refers to the fact that the term UFP is commonly used to describe nanometer-size particles that have not been intentionally produced, but are the incidental products of industrial processes or different types of combustion, and even volcanic activities.10
UFP (or incidental nanoparticles) show more complex chemical composition, irregular shapes, and polydispersed size distribution as compared to engineered particles.12
These particles could exert their effects per se or through a multitude of substances that could be adsorbed on their surfaces. For instance, some engineered NPs exist as nanocrystals composed of a number of compounds such as silicon and metals (quantum dots).13
Carbon fullerenes represent NPs with identical dimensions in all directions (i.e., spherical). They are carbon allotropes rolled up to form closed-cage, hollow spheres. Some of their characteristics such as their small size, large surface area and high reactivity make them interesting in technological and medical fields. They were initially discovered by Kroto, Smalley and Curl (who later won the 1996 Nobel Prize in Chemistry) as a new form of carbon, buckminsterfullerene or C60.5,14,15
Single-walled carbon nanotubes (SWCNTs) typically form convoluted, fibre-like NPs with a diameter below 100nm. Many particle morphologies can be created at the nanoscale, including “flower” and “belt”-like structures.11
Multi-walled carbon nanotubes (MWCNT) are larger and consist of many single-walled tubes stacked one inside the other.16
Carbon nanotubes (CNTs) are distinct from carbon fibres, because the latter consist of strands of layered graphite sheets and are not single carbon molecules. CNTs are reported to be physically very strong and stiff. For example a SWCNT can be up to 10 times as strong as steel and 1.2 times as stiff as diamond.16,17
Close-packed nanotube structures could have a yield strength exceeding 45±7GPa, which is over 20 times the yield strength of typical high-strength steels.17
As would be expected from the above statements, it is now understood that potential occupational and environmental exposure to manufactured NPs is on the increase.
Nanomedicine and the lungThe field of nanomedicine is the science and technology of diagnosing, treating and preventing disease and traumatic injury, of relieving pain, and of preserving and improving human health, using molecular tools and molecular knowledge of the human body. Its objectives encompass monitoring, control, construction, repair, defense and improvement of human biological systems, using engineered devices and nanostructures for medical benefit.18
Nanomedicine involves the best knowledge about the science and technology of intricate systems of nanometre-scale size, with several components, one of which is an active principle, with the whole system leading to a special function connected to the diagnosis, treatment and/or prevention of disease.18
Nanomedicine also includes the identification of new molecular targets, the creation of new synthetic low molecular weight drugs, nanofluidics for targeted synthesis, nanodetection for target identification, the discovery of natural macromolecules, including antibodies, proteins and genes with biological activity and the creation of drug delivery systems (liposomes and nanoparticles–nanopharmaceuticals), promoting disease-specific targeting, in order to thoroughly control the release of the drugs over the desired period of time, or even to supply suitable routes of administration that can reach locations in the body that are traditionally difficult to access, such as the brain.18
Nanotechnology has an enormous potential in the field of human imaging and early recognition of disease, with the tailoring of specific nanoagents for molecular imaging in the context of Magnetic Resonance Imaging, ultrasound, optical imaging, and X-ray imaging.18–23
Other medical areas include gene and oncologic therapy using multicomponent, nanosized delivery vectors. Nanotube drug delivery is promising for cancer therapy with high treatment efficacy and minimum side effects. There is an increasing use of NPs as carrier systems for chemotherapeutic drugs because of the ability to specifically target cancer cells, improve efficacy and reduce systemic toxicity.24
Noble metal NPs can efficiently target several kinds of tumours, as they present highly tunable optical properties that can be adjusted to desirable wavelengths according to their shape and composition with possible uses in tumour targeting, gene silencing and drug delivery; they can also efficiently convert light or radiofrequencies into heat, promoting thermal ablation.25
CNTs can be effective in delivering drugs such as paclitaxel to retard tumour growth in experimental models of cancer.26,27
Solid lipid nanoparticles (SLN) are ideal carriers for weakly soluble drugs, and are alternatives to current colloidal carriers. Inhaled SLN–paclitaxel could represent a potential system for regional delivery to the lungs, with special efficacy on the lymphatic system, fundamental in the progression of lung adenocarcinomas.28
Therefore, targeted nanoparticle delivery to the respiratory system is one of the future trends in nanomedicine, as it can improve drug therapies systemically and locally using advanced drug delivery systems based in more or less complex nanostructures. In the specific area of lung cancer treatment, NPs can revolutionize future chemotherapy options. Other areas of development are the improvement of monoclonal antibodies for lung targeting (attaching antibodies to drug molecules or drug delivery systems), lung imaging, gene delivery, cystic fibrosis treatment (gene therapy and nano-selective and sustained delivery of proteasome inhibitor drugs) and tuberculosis diagnosis and treatment (as macrophage involvement make NPs a perfect drug carrier).28–31
Environmental challenges of exposure to nanoparticlesSoon after the great development and commercial introduction of these materials, some authors raised significant questions about the potential impact on human health and the environment.
In the 1990s, toxicology and epidemiology research on ultrafine aerosols began developing in combination. However, the emerging field of nanotechnology stimulated the actions toward developing a more complete understanding of what unexpected and unanticipated impact nanoscale materials might have on health.12
In recent decades there has been human exposure to nanoscale particles in the form of diesel soot and bulk UFPs from diverse industrial procedures, essentially in the form of combustion-derived UFPs, but also from natural sources such as forest fires and volcanoes.
Exposure to these particles has been associated with pulmonary inflammation, immune changes, and adverse systemic effects including blood hypercoagulability, contributing to undesirable cardiovascular effects.32–35
Consistent with cross-sectional findings and animal studies, there seems to be an association between exposure to air pollution and the progression of atherosclerosis.36 Some studies report the association of particulate matter <2.5 um (PM2.5) and carotid intima-media thickness.37
Oxidative stress, inflammation, induction of a pro-coagulatory state and dysfunction of the autonomic nervous system can enhance respiratory and cardiovascular diseases. Changes in lung function, heart rate, blood pressure and inflammatory state, and also respiratory symptoms, thrombosis, myocardial infarction, arrhythmia, strokes, and death are more often seen in polluted environments, causing shorter life expectancy.38
A lot of the concern related to the exposure to nanomaterials comes from our knowledge from the reports of inhalation of ultrafine particles found in occupational settings and also ultrafine aerosols resulting from combustion. There seems to be an important link between several chronic diseases and the inhalation of UFPs, such as Clara cell carcinomas (polycyclic aromatic hydrocarbons), mesothelioma (asbestos), and berylliosis (beryllium). Some syndromes associated with exposure to aerosols include coal worker pneumoconiosis, emphysema (combustion products), and metal fume fever (zinc, tin, and other transition metals).5
However, the technical requirements for the detection and characterization of nanoparticles in the environment push the limits of modern sampling techniques and instrumentation.5
At present, there are no legal thresholds for nanoparticle number concentrations in ambient air, so local observation networks do not generally monitor them. The development of ambient particle regulations has been limited for technical and practical reasons, such as the lack of standard methods and instrumentation, and the uncertainty about repeatability and reproducibility of measurements.39
Assessment of the risk associated with nanoparticles requires knowledge about the ability of a material to reach a sensitive site of action, and the type and magnitude of the resultant response at the sensitive site.5
NanotoxicologyThe lung is the primary and probably the most important target of nanomaterials, but NPs can enter the circulation and migrate to various organs and tissues, where they can build up and injure organ systems that are sensitive to oxidative stress. The types of toxicological response will probably vary between molecular and nano-sized forms.
The size of the NPs suggests that the physiological responses could be of an immune or inflammatory nature. These adverse effects may not follow a classic dose-response curve, and can display high unpredictability within the population, potentially dependent on individual sensitivity.5
Nanoparticle toxicity is extremely complex and multifactorial and depends on a multiplicity of physicochemical properties such as size and shape, as well as surface properties (charge, area, and reactivity). Ultrafine or nanosize range (<100nm) particles seem to be more toxic on a mass-based exposure metric compared to larger particles of identical chemical composition. Also, particle surface area dose is a better predictor of the toxic and pathological responses to inhaled particles than particle mass dose.9,40
Differences in physico-chemical properties between NPs and larger particles determine their behaviour as aerosol, their biodistribution following translocation from the portal of entry, their cellular interactions and effects. Secondary organs are usually affected differently from the primary target of these particles.27
In 1990, the Journal of Aerosol Science published two of the first cornerstone papers on a higher than expected effect on lung inflammation patterns in rats exposed to NPs, effects that could not be predicted by just taking the chemical composition and the inhaled amounts of the particles into account.41–43
One of the first important assumptions, that is still of great importance, is that NPs have the potential to show previously unrecognized biological behaviour.43
A major report concerning the uncertainties of nanotechnologies was published in 2004 by the Royal Society and the Royal Academy of Engineering.44 This was one of the first reports to highlight the potential risks to health and the environment that may arise from exposure to nanomaterials, especially NPs (which included nanomaterials such as nanotubes). Since then, more than fifty national and international reviews carried out by government departments, industry associations, insurance organizations and researchers have considered nanoparticle risk issues.
A workshop co-sponsored by the National Science Foundation and the US Environmental Protection Agency has identified a number of potential risks regarding manufactured NPs, such as exposure assessment of manufactured NPs; toxicology of manufactured NPs; the ability (or not) to extrapolate manufactured nanoparticle toxicity using existing particle and fibre toxicological databases; environmental and biological fate, transport, persistence, and transformation of manufactured NPs, recyclability and overall sustainability of manufactured nanomaterials.45
The ability of absorbed particles to generate local toxic effects at the site of initial deposition as well as very significant systemic toxic responses shows how dangerous they can be in real-life settings. The potential for adverse health effects may arise from direct exposure to intentionally produced nanomaterials and/or byproducts associated with their applications.9
Toxicological assessment of manmade nanomaterials requires information about the route (inhalation, oral, dermal) of exposure, as well as their complete physicochemical characterization of them in order to provide thorough information. The most common scenarios for human exposure to NPs are occupational, environmental and consumer ones.
Inhalation hazards of nanoparticlesOne of the most widespread routes of human exposure to airborne NPs is inhalation in the workplace and the environment.
As seen before, at present there are large numbers of nanomaterials; as their technological and toxicological properties vary considerably, so will their risk profiles.46 We are now able to consider that the extensive and heterogeneous group of NPs of diverse scale constitutes an inhalation hazard of unknown potential.
The deposition of NPs in the respiratory tract is determined essentially by the particle aerodynamic or thermodynamic diameter (depending on particle size).11
According to the classical model developed by the International Commission on Radiological Protection (ICRP), the probability of nanoparticles reaching the alveoli peaked at a size of approximately 20nm, with lower probabilities of deposition in the alveoli for both smaller and larger nanoparticles. Nanoparticle deposition, in particular for smaller particles, is governed by Brownian movements.12
There are still issues that have not yet been fully resolved about how exposure to NPs can be thoroughly measured and quantified; they are usually described as mass concentration (units mgm−3); number concentration (units per m−3) and surface area concentration units (m2m−3).
As stated before, the possible health effects arising from exposure to NPs may be better correlated with surface area, rather than with mass concentration.6,16
NPs have some essential properties that could be directly related to their pathogenicity:
- -
As particles less than 100nm, they may have more toxicity than larger sized particles.
- -
Generally they are considered as fibre shaped, and so might behave like some other pathogenic fibres (asbestos, man-made fibres).
- -
As most of the NPs have an essentially graphitic constitution, they are expected to be biopersistent in biological settings, such as the respiratory system.16
Commercial NPs could also contain some impurities, a common result of the synthesis process, such as metals (Co, Fe, Ni, and Mo), organic compounds, and support material.16
Smaller particles are likely to be more aggressive to the lung than larger particles; particles with more inert surfaces may be aggressive, exerting their effects on cells by reason of having a large surface area. Particles with more reactive surfaces can affect cells without necessarily having large surface areas.16
Shape, biopersistence, presence of transition metals and the power to generate reactive oxygen species also explain the potential for lung damage. In fact, some of the main experimental studies in rodents and cell cultures have shown that the toxicity of UFPs or NPs is greater than that of the same mass of larger particles with a similar chemical composition, posing specifically a higher respiratory and systemic health threat.11
At equivalent mass doses, insoluble ultrafine particles cause more damage than larger particles of a similar composition in terms of pulmonary inflammation, tissue damage, and lung tumours.11
From the alveoli, NPs have the potential to enter the bloodstream from the lungs and even translocate to other organs.11 For instance, biokinetic studies show that inhaled NPs can translocate via olfactory neurons from the nose to the Central Nervous System.40
The biokinetics of NPs in the body varies, depending on the portal of entry. The same NPs entering the lung (via inhalation or intratracheal instillation) or intravenously, interact with different biological media and will receive different secondary coatings, affecting nanoparticle biodistribution to target organs.27
At present, carrying out risk assessment of NPs can only be done sensibly on a case-by-case basis.6
Most of the studies about the effects of respiratory exposure to NPs involve pulmonary models and are performed through instillation, aspiration and inhalation of carbon nanotubes (the most studied NPs) in rodent species.
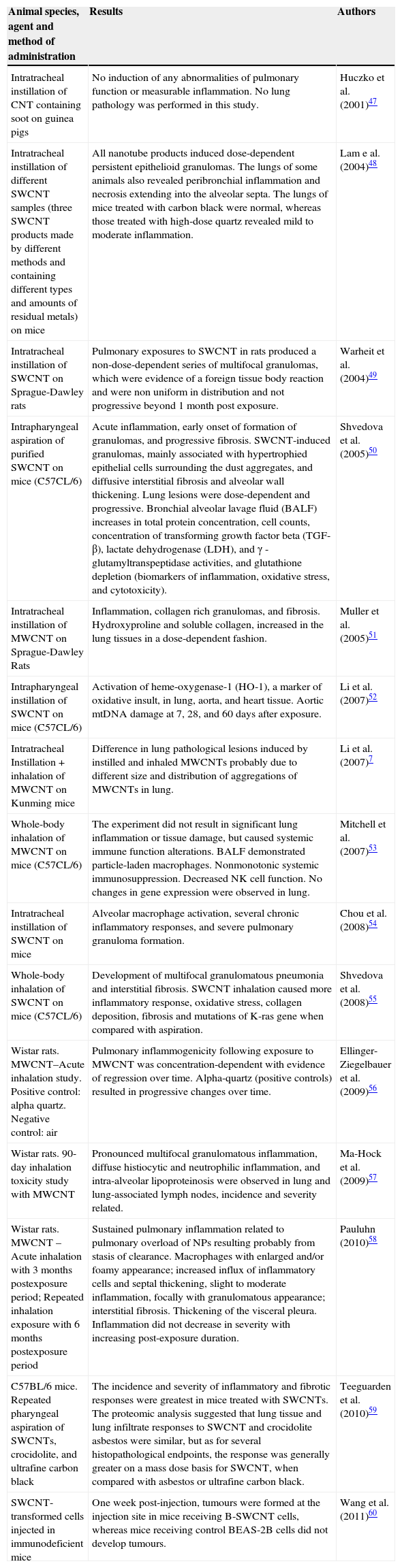
Table 1 summarizes some of the main in vivo investigations regarding the respiratory effects of carbon nanotubes.
In vivo investigations of carbon nanotube toxicity.
| Animal species, agent and method of administration | Results | Authors |
|---|---|---|
| Intratracheal instillation of CNT containing soot on guinea pigs | No induction of any abnormalities of pulmonary function or measurable inflammation. No lung pathology was performed in this study. | Huczko et al. (2001)47 |
| Intratracheal instillation of different SWCNT samples (three SWCNT products made by different methods and containing different types and amounts of residual metals) on mice | All nanotube products induced dose-dependent persistent epithelioid granulomas. The lungs of some animals also revealed peribronchial inflammation and necrosis extending into the alveolar septa. The lungs of mice treated with carbon black were normal, whereas those treated with high-dose quartz revealed mild to moderate inflammation. | Lam e al. (2004)48 |
| Intratracheal instillation of SWCNT on Sprague-Dawley rats | Pulmonary exposures to SWCNT in rats produced a non-dose-dependent series of multifocal granulomas, which were evidence of a foreign tissue body reaction and were non uniform in distribution and not progressive beyond 1 month post exposure. | Warheit et al. (2004)49 |
| Intrapharyngeal aspiration of purified SWCNT on mice (C57CL/6) | Acute inflammation, early onset of formation of granulomas, and progressive fibrosis. SWCNT-induced granulomas, mainly associated with hypertrophied epithelial cells surrounding the dust aggregates, and diffusive interstitial fibrosis and alveolar wall thickening. Lung lesions were dose-dependent and progressive. Bronchial alveolar lavage fluid (BALF) increases in total protein concentration, cell counts, concentration of transforming growth factor beta (TGF-β), lactate dehydrogenase (LDH), and γ - glutamyltranspeptidase activities, and glutathione depletion (biomarkers of inflammation, oxidative stress, and cytotoxicity). | Shvedova et al. (2005)50 |
| Intratracheal instillation of MWCNT on Sprague-Dawley Rats | Inflammation, collagen rich granulomas, and fibrosis. Hydroxyproline and soluble collagen, increased in the lung tissues in a dose-dependent fashion. | Muller et al. (2005)51 |
| Intrapharyngeal instillation of SWCNT on mice (C57CL/6) | Activation of heme-oxygenase-1 (HO-1), a marker of oxidative insult, in lung, aorta, and heart tissue. Aortic mtDNA damage at 7, 28, and 60 days after exposure. | Li et al. (2007)52 |
| Intratracheal Instillation+inhalation of MWCNT on Kunming mice | Difference in lung pathological lesions induced by instilled and inhaled MWCNTs probably due to different size and distribution of aggregations of MWCNTs in lung. | Li et al. (2007)7 |
| Whole-body inhalation of MWCNT on mice (C57CL/6) | The experiment did not result in significant lung inflammation or tissue damage, but caused systemic immune function alterations. BALF demonstrated particle-laden macrophages. Nonmonotonic systemic immunosuppression. Decreased NK cell function. No changes in gene expression were observed in lung. | Mitchell et al. (2007)53 |
| Intratracheal instillation of SWCNT on mice | Alveolar macrophage activation, several chronic inflammatory responses, and severe pulmonary granuloma formation. | Chou et al. (2008)54 |
| Whole-body inhalation of SWCNT on mice (C57CL/6) | Development of multifocal granulomatous pneumonia and interstitial fibrosis. SWCNT inhalation caused more inflammatory response, oxidative stress, collagen deposition, fibrosis and mutations of K-ras gene when compared with aspiration. | Shvedova et al. (2008)55 |
| Wistar rats. MWCNT–Acute inhalation study. Positive control: alpha quartz. Negative control: air | Pulmonary inflammogenicity following exposure to MWCNT was concentration-dependent with evidence of regression over time. Alpha-quartz (positive controls) resulted in progressive changes over time. | Ellinger-Ziegelbauer et al. (2009)56 |
| Wistar rats. 90-day inhalation toxicity study with MWCNT | Pronounced multifocal granulomatous inflammation, diffuse histiocytic and neutrophilic inflammation, and intra-alveolar lipoproteinosis were observed in lung and lung-associated lymph nodes, incidence and severity related. | Ma-Hock et al. (2009)57 |
| Wistar rats. MWCNT – Acute inhalation with 3 months postexposure period; Repeated inhalation exposure with 6 months postexposure period | Sustained pulmonary inflammation related to pulmonary overload of NPs resulting probably from stasis of clearance. Macrophages with enlarged and/or foamy appearance; increased influx of inflammatory cells and septal thickening, slight to moderate inflammation, focally with granulomatous appearance; interstitial fibrosis. Thickening of the visceral pleura. Inflammation did not decrease in severity with increasing post-exposure duration. | Pauluhn (2010)58 |
| C57BL/6 mice. Repeated pharyngeal aspiration of SWCNTs, crocidolite, and ultrafine carbon black | The incidence and severity of inflammatory and fibrotic responses were greatest in mice treated with SWCNTs. The proteomic analysis suggested that lung tissue and lung infiltrate responses to SWCNT and crocidolite asbestos were similar, but as for several histopathological endpoints, the response was generally greater on a mass dose basis for SWCNT, when compared with asbestos or ultrafine carbon black. | Teeguarden et al. (2010)59 |
| SWCNT-transformed cells injected in immunodeficient mice | One week post-injection, tumours were formed at the injection site in mice receiving B-SWCNT cells, whereas mice receiving control BEAS-2B cells did not develop tumours. | Wang et al. (2011)60 |
Many of the most pressing health and safety concerns regarding NPs and nanotechnologies come from the lack of knowledge about levels of occupational and other types of exposure during their production and use.61
Among the particles with potential respiratory risks, CNTs are one of the specialized structures of engineered NPs that are widespread. Discovered more than 20 years ago, they have increasing potential uses in biomedical, aeronautic, and industrial fields due to their unique conductive and electrochemical properties.59
As seen before, CNTs are classified according to their structure: single-walled carbon nanotubes (SWCNT) and multi-walled carbon nanotubes (MWCNT).
Nanotubes can have features of both NP and conventional fibres. The literature currently available suggests that CNT may have toxic effects beyond those predictable for their mass exposure. For instance, they have more adverse effects than the same mass of NP carbon and quartz, a commonly used comparator amongst harmful inhalable particles.16
CNTs can induce oxidative stress and inflammation, and several studies imply that they could cause granuloma formation and fibrogenesis.16
In occupational contexts, CNTs should be considered in the same way as other biopersistent fibres in the workplace, with implications for at least similar approaches to control and assessment.16
It would appear that the main mechanism of engineered nanomaterial toxicity is related to oxidative stress, caused by the activation of responsive transcription factors. Chronic inflammation and oxidative stress observed during and after exposure can induce adverse health effects such as fibrosis, genotoxicity and cancer caused by fibres or secondary mutation.62
One of the first studies on the subject of CNTs exposure was performed by Lam et al.48 In this study mice were instilled intratracheally with 0, 0.1, or 0.5mg of carbon nanotubes, a carbon black negative control, or a quartz positive control, and lung pathology studied 7 or 90 days after exposure. All nanotube products induced dose-dependent epithelioid granulomas and, in some cases, interstitial inflammation, which was more pronounced in the 90-day group. Some animals had peribronchial inflammation and necrosis, extending to the alveolar septa. On a same weight basis, when CNTs reach the lungs, they are much more toxic than carbon black and can be more toxic than quartz.48
Inhalation studies are able to provide more information and reproducibility of occupational and environmental risks. However, instillation studies are less complex and cheaper, so they could represent a form of screening for the potential harm and toxicity of NPs.62
In the experiments where intratracheal instillation of NPs was performed, more pronounced and severe effects were observed, when compared with inhalation studies.62,63
CNTs have toxicologically significant structural and chemical similarities to asbestos, and experiments have shown that they cause pulmonary inflammation, granuloma formation and fibrosis after entering the respiratory system of rodents, as observed after exposure to asbestos. Some studies confirm for MWCNTs a well established asbestos-like pathogenicity that is associated with long fibres.59,64
In addition, the impact of some impurities, such as metals, present in some MWCNTs cannot be underestimated in the forms in which the lung could be affected.65
According to Pacurari et al., the fibrous characteristics of MWCNT, their durability and their ability to generate reactive oxygen species at low levels in cellular systems may contribute to the initiation and progression of asbestos-like pathological responses.66
Shvedova et al. demonstrated that SWCNT inhalation resulted in mutations of K-ras gene locus in the lung of C57BL/6 mice. This is one of the mutated genes that can be implicated in pulmonary tumourigenesis.55
Aerosolized inhalation in animal studies supports a common sequence of biological events following single CNT exposure: important acute phase inflammation similar to a foreign body response, followed by formation of multifocal granulomas, and early onset fibrosis.59
MWCNTs and other carbon NPs in fine (<2.5μm) particulate matter (PM) aggregates have been related to the combustion of methane, propane, and natural-gas flames of some stoves; indeed, indoor and outdoor fine PM samples were reported to contain significant fractions of MWCNTs.
A very recent study from Teeguarden et al. used high sensitivity based proteomics – HPLC–FTICR–MS (high performance liquid chromatography/Fourier transform ion cyclotron resonance mass spectrometry) to assess some of the major differences in exposure to three materials – SWCNT, asbestos, and ultrafine carbon black (UFCB).59 Rodent exposure to SWCNT led to a significantly greater inflammatory response, when compared with crocidolite asbestos and UFCB, with an increase in polymorphonuclear neutrophils (PMNs) and total cell count of bronchoalveolar lavage fluid (BALF). Also, moderate multifocal inflammation was present in all lungs from SWCNT exposed mice, with granuloma formation near bronchioles and adjacent alveoli consisting of round clusters of large macrophages and multinucleated giant cells. Statistically significant differences in some cytokines (TARC, IL-12 and MDC) were also seen, proving the high inflammogenic potential of SWCNT. In addition, the proteomic analysis conducted by the authors supports the conclusion that lung tissue and lung infiltrate responses were generally greater on a mass dose basis for SWCNT.
The potential for particles to cause fibrotic reactions within the lung depends on the particle size, composition, surface activity, and retained dose. Particles containing certain transition metals have a greater capacity to generate reactive oxygen species, in addition to those already generated by inflammatory neutrophils and activated alveolar macrophages.58
Recently, Wang at al. demonstrated that chronic exposure to SWCNT can produce malignant transformation of human lung epithelial cells. Also, SWCNT-transformed cells injected in immunodeficient mice led to tumour growth at the injection site in mice receiving SWCNT-transformed BEAS-2B cells, whereas mice receiving control BEAS-2B cells did not develop tumours, showing also the potential role of p53 in this process.60
Like other areas of knowledge regarding nanotechnologies, studies of the carcinogenic potential of carbon nanotubes are still in the early stages, but there are some data suggesting that these structures are not risk free, and can be widely dependent on several other physico-chemical and biological characteristics, and also specific composition and type and size of impurities.3
Also, fullerenes (NPs with identical dimensions in all directions) following exposure via the pulmonary route are capable of eliciting localized responses that are pro- or anti-inflammatory in nature, with the type of response initiated likely to be reliant on the fullerene in question, exposure method and the dose used. However, inhalation studies regarding the effects of fullerenes are still limited.6
Fullerene toxicity probably involves an oxidant response, suggesting the potential of fullerenes to cause oxidative stress and related consequences (such as inflammation or genotoxicity). Generally, the greater the water solubility exhibited by a fullerene sample, the lower the toxicity associated with exposure.6
In addition, recent studies in murine models prove that titanium dioxide (TiO2) or gold (Au) NPs can interfere with the modulation of the asthmatic response regarding diisocyanate induced asthma, as they can aggravate pulmonary inflammation and airway hyperreactivity.67
There is still a shortage of publications addressing the in vivo, real world effects of nanoparticle exposure. However, some of these are very worrying; for instance, Chinese workers exposed to polyacrylate consisting of NPs in a print plant have shown shortness of breath, and the same clinical findings of pleural effusion and pericardial effusion. The study of these workers revealed nonspecific pulmonary inflammation, pulmonary fibrosis and foreign-body granulomas of the pleura; BALF elicited increased lymphocytes and neutrophil leukocytes. Two young patients subsequently died from respiratory failure.68
Conclusions and future trendsRespiratory exposure to NPs can cause important adverse respiratory effects, such as multifocal granulomas, peribronchial inflammation, progressive interstitial fibrosis, chronic inflammatory responses, collagen deposition, oxidative stress, pleural lesions and gene mutations, at least in experimental animal studies.
At this point in time, it is fundamental to know more about the toxicological effects of NPs, to address the increased concern of potentially harmful public and occupational exposures.27
A very wide range of endpoints have to be considered when testing potential risks derived from NPs. Hazards should be tested according to their potential routes within the human body.
According to Oberdörster in a recent paper regarding the safety assessment for nanotechnology, although many of the current engineered nanomaterials with a potential for human exposure are not likely to induce significant adverse effects, some could cause an asbestos-type disaster if it is not controlled.27
There is, therefore, an urgent need for the development of criteria for extrapolating toxicological data in biological systems in order to predict the risk of adverse outcomes in humans.65
Not only traditional tests, but also newer models reflecting the permanent evolution of nanotoxicology as an emerging field, should be used to shed light on the mechanisms of NP toxicity. The combination of in vitro and in vivo tests should contribute to hazard assessment in the future. A multidisciplinary team approach is fundamental to addressing respiratory human risks related with Nanotechnology.
At present, there are several extremely relevant attempts currently under way in order to formulate a science-based risk management research framework. One of them is the US. National Nanotechnology Initiative/Environmental, Health, and Safety Research Strategy; the main research needs to include, among other points, the development of measurement tools for the determination of physico-chemical properties of engineered nanomaterials (ENMs), their detection and monitoring in realistic exposure media and conditions during the life cycle, the evaluation of transformations of ENMs in relevant media, the further assessment of biological responses, the better understanding of the processes and factors that determine exposures to nanomaterials, the identification of population groups exposed to ENMs and their health surveillance, and the development of appropriate, reliable, and reproducible assays and models to predict human responses to ENMs.
With appropriate strategies that integrate risk assessment into decision-making frameworks for risk management, and incorporate and standardize risk communication within the risk management framework, better esults should be expected in the future.2
Now is the time to promote, on a global scale, an in-depth discussion and evaluation of the human and environmental risks of these new materials; as stated by Maynard et al.,43 these resources are “merely the vanguard of a new era of complex materials, where novel and dynamic functionality is engineered into multifaceted substances. If we are to meet the challenge of ensuring the safe use of this new generation of substances, it is time to move beyond “nano” toxicology and toward a new toxicology of sophisticated materials.”
Ethic disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.