We report an extraordinary case of collision tumor consisting of a lung adenocarcinoma and a metastatic adenoid cystic carcinoma in a 56 year-old man. He was diagnosed with a pulmonary nodule 11 years after treatment of an adenoid cystic carcinoma of the right maxillary sinus. A non-small cell carcinoma was observed when a transbronchial biopsy was performed. The other component of the nodule was only diagnosed with pathological examination of the resection specimen.
Descrevemos um caso único de tumor de colisão constituído por um adenocarcinoma de pulmão e uma metástase dum carcinoma adenóide cístico em um homem de 56 anos de idade. Ao doente foi diagnosticado um nódulo pulmonar 11 anos após o tratamento de um carcinoma adenóide cístico do seio maxilar direito. O carcinoma de pulmão de não pequenas células foi observado no momento da realização de uma biópsia transbrônquica. O outro componente do nódulo foi diagnosticado depois do exame histológico do material ressecado.
Collision tumors are a rare condition in which two histologically different malignant neoplasms, originating from two separate primary sites, intermix with one another. The two malignancies may originate from the same organ or occur as metastases from other sites. There is no histological admixture or intermediate-transition cell population zone. These tumors are difficult to diagnose preoperatively and pathological identification of the dual components is often the only way to make a correct diagnosis.1
Adenoid cystic carcinoma (ACC) is a malignant tumor that is commonly classified with the salivary gland tumors, although it may arise at any site where mucous glands exist. This tumor exhibits a unique malignant profile, which is characterized by slow growth and high propensity to systemic metastases. The lung is the most common site of metastasis, as pulmonary metastases have been reported in more than 38% of patients with ACC of the head and neck. Most patients with metastatic disease are relatively asymptomatic and may remain so for long periods.2,3
Several case reports have been published in the literature, which describe a primary pulmonary collision tumor consisting of large-cell carcinoma and adenocarcinoma4 or squamous cell carcinoma and T-cell lymphoma.5 To our knowledge, this is the first report that describes a case of collision cancer in the lung consisting of a lung adenocarcinoma and a metastasis of an ACC diagnosed with immunohistochemical techniques performed after surgery.
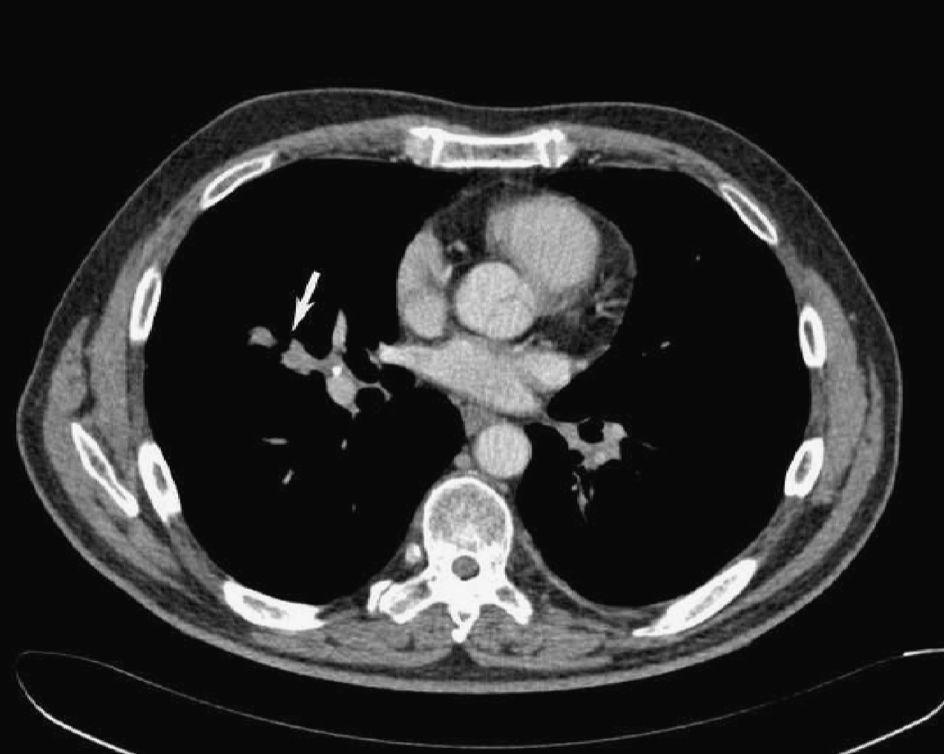
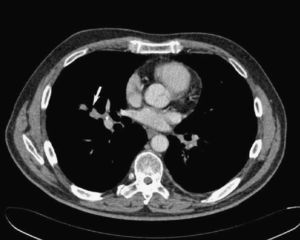
Case reportA 56-year-old man with a previous history of adenoid cystic carcinoma of the right maxillary sinus (pT4N0Mx) that had been treated by right radical hemimaxillectomy and radiotherapy 11 years earlier was admitted to our institution after referral from his oncologist. During the regular follow-up, a computed tomography (CT) scan showed a 2.5cm diameter nodule, with irregular morphology in the middle lobe, which was in contact with the middle lobe brochus and right inferior lobar artery (Fig. 1). A transbronchial biopsy with bronchoscopy was performed showing an epithelial neoplastic cell proliferation with large cytoplasms and hyperchromatic nuclei. Neoplastic cells expressed Cytokeratin AE1/AE3, Cytokeratin 7 and TTF-1. With these features, non-small cell carcinoma with immunohistochemical stigmas of adenocarcinoma was diagnosed. A positron emission tomography (PET) demonstrated a focus of increased FDG uptake in the right hilum contacting with the middle lobe.
It was necessary to perform a middle-lower bilobectomy as the nodule was located in the hilum of the middle lobe and affected the major fissure. Mediastinal lymph node dissection was performed including stations 7, 8, 9 and 4R. The postoperative course was uneventful, and the patient was discharged on day 9 after the operation.
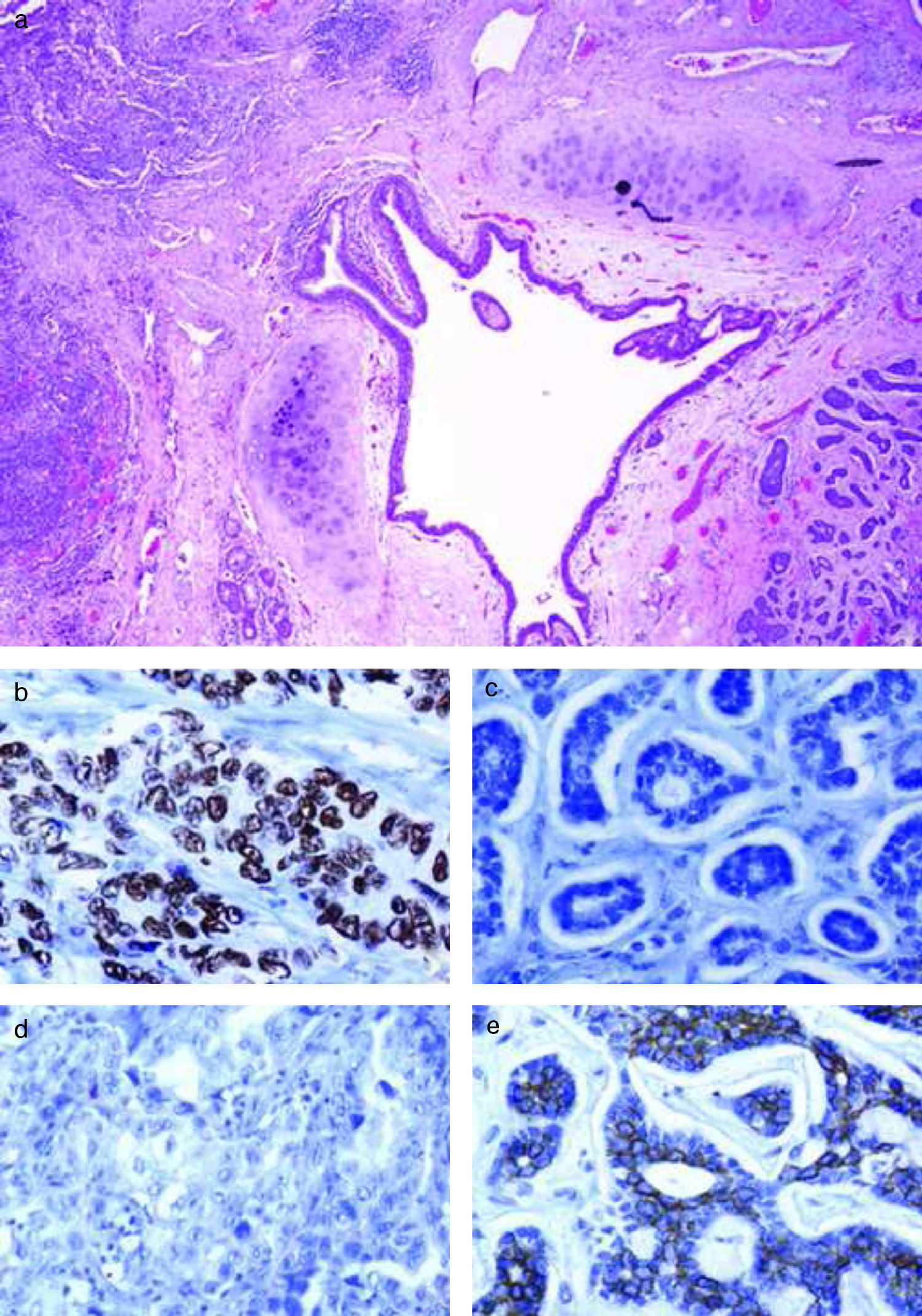
Histologically, the nodule located in the middle lobe was a collision tumor of 2.5cm diameter formed by a lung adenocarcinoma with a poorly differentiated grade (1.1cm×1cm) and a metastatic ACC (1.5cm×1cm) 0.2cm away from the primary tumor. We did not observe histological admixture or an intermediate cell population zone (Fig. 2a). A subpleural nodule of ACC was also observed in the right lower lobe (0.5cm). There was no evidence of vascular invasive tumor, the resection bronchial margin was negative and all the lymph nodes were free (Fig. 2). In the immunohistochemical work-up, one area consisted of glandular neoplasic proliferation with poorly differentiated areas and large cells with severe cytologic atypia TTF-1 positive (Fig. 2b) and C-kit (CD117) negative (Fig. 2d). The other area was formed by basophil epithelial nests with the presence of mucoid material inside. These cells showed a moderate grade of cytologic atypia and were positive for C-kit (Fig. 2e) and negative for TTF-1 (Fig. 2c).
(a) Section of the collision tumor stained with hematoxilyn and eosin. We can observe the lung adenocarcinoma on the left side of the bronchial lumen and the adenoid cystic carcinoma on the right; objective magnification 20×. (b) Immunohistochemical detection of TTF-1 was positive in the lung adenocarcinoma; objective magnification 400×. (c) Immunostaining with TTF-1 in the adenoid cystic carcinoma was negative; objective magnification 400×. (d) Immunohistochemical detection of C-kit was negative in the lung adenocarcinoma; objective magnification 400×. (e) C-kit expression in the adenoid cystic carcinoma with a basal immunostaining; objective magnification 400×.
The patient is alive and disease-free without any further treatment 17 months following surgery.
DiscussionThe occurrence of multiple malignancies in the same anatomical site in organs such as the thyroid, breast and lymph nodes has been previously described.6 In the lung, single cases of bronchogenic carcinoma have been unexpectedly found when pulmonary resection was performed for metastatic lung cancer.7 Nevertheless, the occurrence of synchronous colliding tumors remains an extremely uncommon condition with a very limited number of cases having been published in the literature.
ACC is a rare form of malignant neoplasm that usually originates within the major and minor salivary glands of the head and neck. Clinically, this tumor presents insidiously and is generally advanced when diagnosed. ACC seldom metastasizes to regional lymph nodes. Nevertheless, a distant spread to the lungs and bones occurs frequently. The distant metastasis can cause death as long as 10–20 years after initial treatment.8 In our case, as described in the literature, metastasis appeared in the lung 11 years after treatment. Nevertheless we did not suspect the existence of an ACC metastasis inside the nodule because there were no local recurrences during the follow-up period and we found a positive transbronchial biopsy for non-small cell carcinoma.
Immunohistochemical study was important for the final diagnosis; part of the nodule was negative for TTF-1 and positive for C-kit, which is a transmembrane type III receptor tyrosine kinase that has recently been reported to be expressed in ACC.9 C-kit is activated by binding of its ligand, stem cell factor. Binding of stem cell factor initiates a phosphorylation cascade that ultimately leads to activation of various transcription factors that regulate apoptosis, cell differentiation and proliferation. Kit protein expression is important in the development of normal human tissues and in many human neoplasms including mastocytosis, gastrointestinal stromal cell tumors, melanoma, breast cancer, gynecologic cancers, thyroid neoplasms, etc.10,11 Recently, Kit expression has been identified in several types of salivary gland tumors. In these tumors, kit expression has been most extensively documented in adenoid cystic carcinomas with an expression frequency ranging from 67 to 100.12
If we consider the origin of ACC, we must distinguish metastatic ACC from primary ACC of the lung. Pulmonar ACC is a malignant tumor arising in the tracheobronchial glands distributed in the airway submucosa, with a similar morphology to ACC arising in the salivary glands. Because of the site of origin, pulmonary ACC is more common in the central bronchi than in the segmental bronchi. Reports of ACC originating in the peripheral lung are rare. In addition, in cases of occurrence in the periphery, lung metastases from a salivary gland tumor must be ruled out.13 In our case, the characteristics we observed gave us the final diagnosis of a metastatic ACC. These characteristics were: (1) The obvious difference in the histological pattern between the two tumors. Moreover, we did observe no histological admixture or an intermediate cell population zone between both tumors. (2) The different immunohistochemical expression of both tumors for C-kit and TTF-1. (3) The existence of another subpleural nodule in the right lower lobe. (4) The oncology history of the patient.
In conclusion metastasis in ACC can manifest itself very late, and thus, long-term follow-up and a high index of suspicion is necessary to diagnose them early. This was observed in the present case. We would like to emphasize the role of detailed histopathologic analysis and the use of immunohistochemistry in better identifying lung neoplasms.
Conflict of interestThe authors declare that they have no conflict of interest.