Well-differentiated fetal adenocarcinoma (WDFA) is a very uncommon malignant tumor originating in the lung. This report describes the case of a 38-year-old woman with a WDFA treated by surgery. The malignancy is low grade and associated with a good prognosis, and so it is important for clinicians to be aware of and to identify this rare variant of adenocarcinoma.
O adenocarcinoma fetal bem diferenciado (WDFA, de acordo com a sigla em inglês) é um tumor maligno no pulmão muito invulgar que tem origem no pulmão. Este relatório descreve o caso de uma mulher de 38 anos com WDFA tratada através de cirurgia. A malignidade é de baixo grau e está associada a um bom prognóstico e, por isso, é importante que os clínicos estejam atentos e identifiquem esta variante rara de adenocarcinoma.
Fetal Adenocarcinoma is a very uncommon malignant tumor originating in the lung, and was first described by Kradin et al.1 as a subtype of pulmonary blastoma, which resembled the epithelial component of the fetal lung without sarcomatous contingent.
In 1984, the term fetal adenocarcinoma was introduced by Kodama et al.2 14 years later Nakatani et al. identified 2 groups: well differentiated occurring in young women and with a good prognosis and poorly differentiated with a similar prognosis to classical non-small cell carcinoma.3 Fetal adenocarcinoma has been considered in the WHO classification since 1999 as a solid adenocarcinoma with mucin production. However, a new international multidisciplinary classification, which focused on lung adenocarcinoma to standardize terminology and improve treatment and predict prognosis, does not consider fetal adenocarcinoma as a solid adenocarcinoma with mucin production but as a variant of invasive adenocarcinoma.4
We (The authors) report a case of a 38-year-old female patient with WDFA, and discuss the unusual features of this type of tumor.
Case reportA 38 year old woman presented with a one year history of dyspnea for which she was put on a short-acting bronchodilator with no further testing, in particular no chest X-ray considering she was in the early stages of pregnancy. Two months after delivery, she reported an aggravation of her dyspnea with no other respiratory or extra respiratory signs and was examined two months later. She had no significant past medical history; she had no history of smoking. The physical examination was normal.
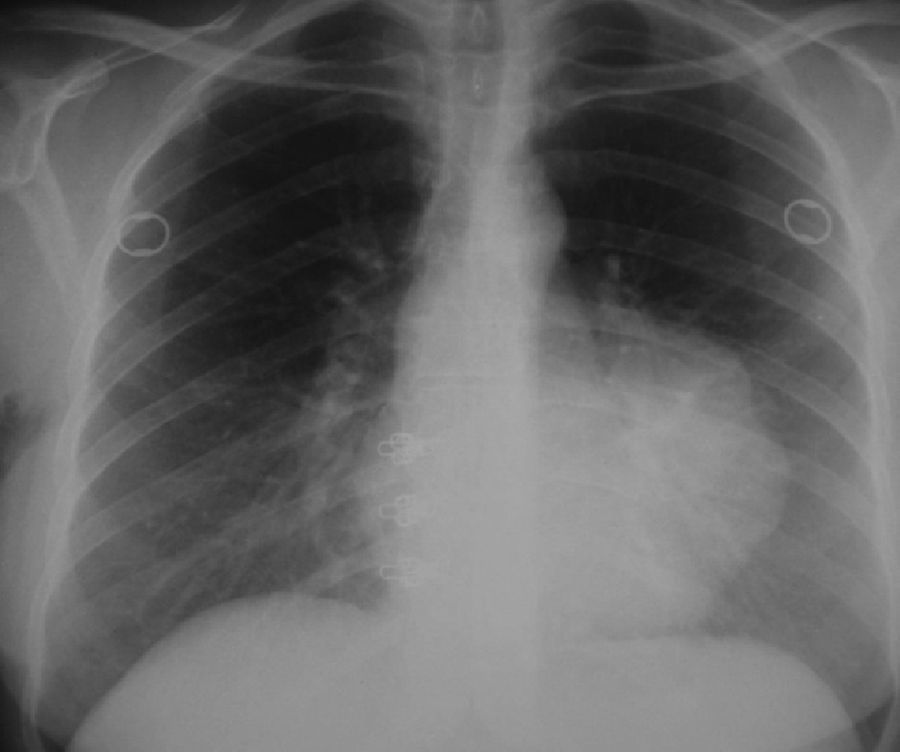
A chest X-ray (Fig. 1) showed a hilar and paracardial left opacity with a well defined border and internal margin which extended into the mediastimum.
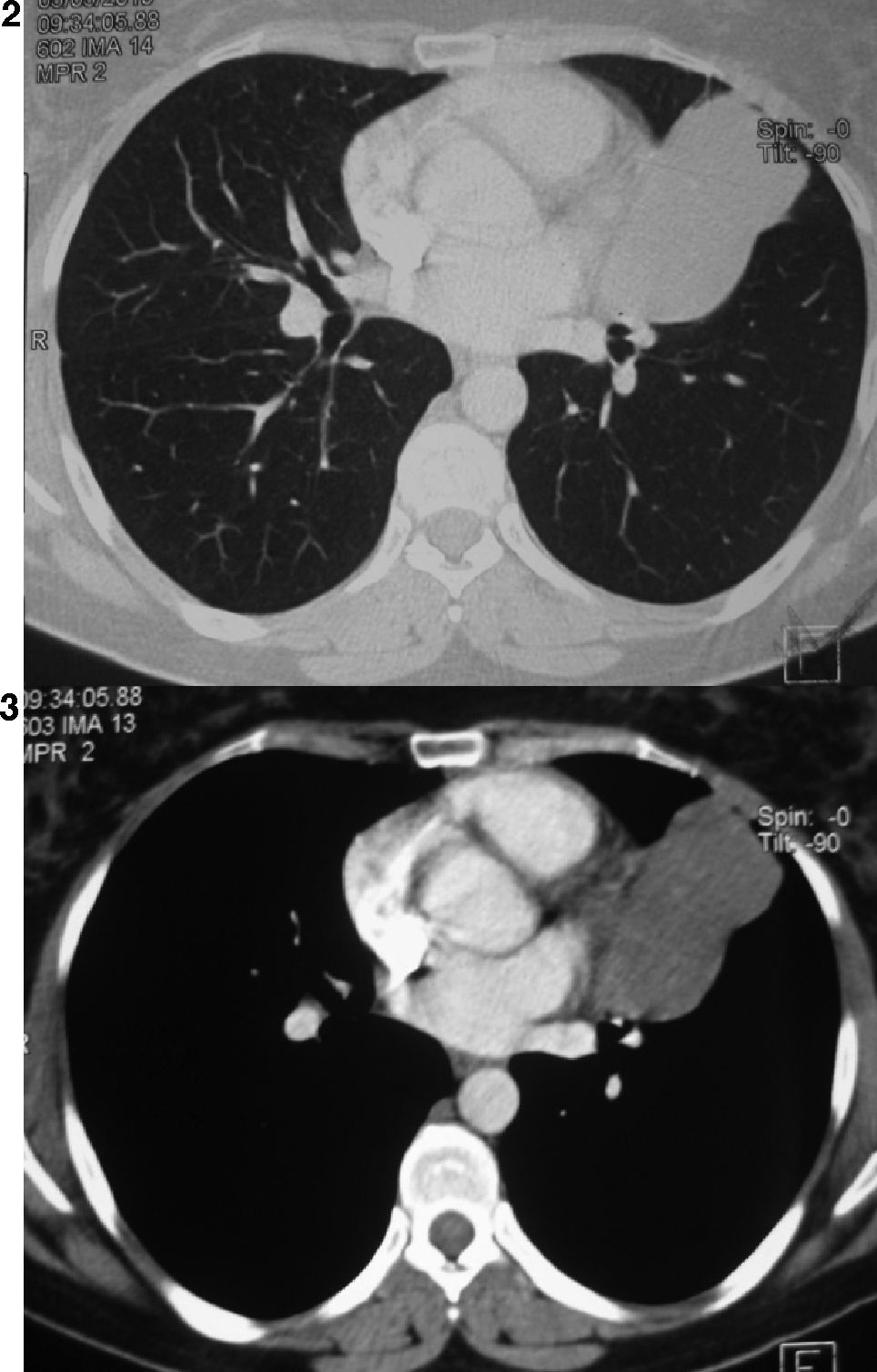
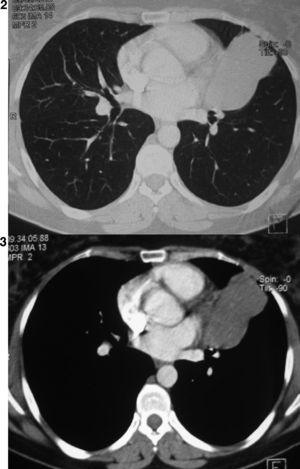
A computed tomography scan (Figs. 2 and 3) revealed a partially cystic heterogeneous mass, forming at the lingular bronchi and then developing in intrathoracic without mediastinal lymphadenopathy or pleural effusion.
Bronchoscopy confirmed a whitish lingular lesion at the orifice, with total occlusion of the airway lumen.
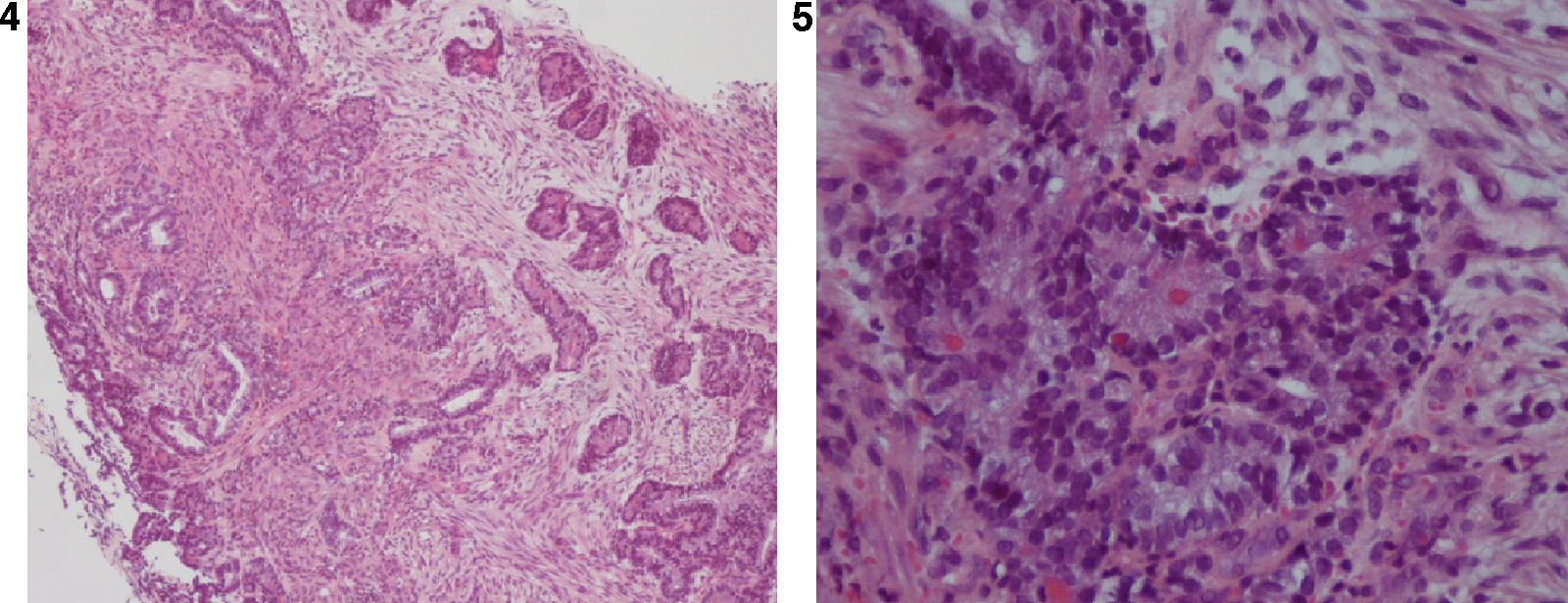
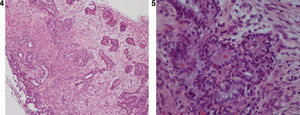
Microscopic examination of an endobronchial biopsy (Figs. 4 and 5) showed an obviously malignant tumor process which was extensively ulcerated on the surface. It was made up of malignant glandular cells growing in tubules and papillary structures, sometimes reproducing endometrioid differentiation. These malignant cells had prominent clear cytoplasm, and squamoid morules were present. Some of the lumen of the glands were empty, others contained eosinophilic material. The dividing stroma was fibrous. Large areas of necrosis were observed.
The patient was assessed clinically at stage T3N0M0. Thoracotomy was performed and the patient underwent a superior left lobectomy with lymphadenectomy. The tumor measured 6cm at the widest diameter. Microscopic examination confirmed the description above.
DiscussionLung tumors resembling the fetal lung are a very uncommon primitive malignant tumor originating in the lung. They include pulmonary blastoma and fetal adenocarcinoma.4 The incidence of this malignant tumor has been estimated at 0.5% of all primary lung tumors.5
In the series of Kodama et al., all the patients were elderly males. The majority died of their tumor. Koss et al. reported a series with better survival where almost all the patients were female. In 1990, Natakatani et al. identified subcategories of fetal type adenocarcinoma where the prognosis was good, specifically occurring among woman.
In 1998 Natakatani et al. identified 2 groups of fetal adenocarcinoma: WDFA occurring in young women, generally non smokers, which had a good prognosis, also called endodermal tumor resembling the fetal lung, and poorly differentiated fetal adenocarcinoma with a similar prognosis to classical non-small cell carcinoma.
Histologically, the WDFA element characteristically demonstrates glandular elements with tubules composed of glycogen-rich, non-ciliated cells that resemble fetal lung tubules and squamoid morules may be seen with clear nuclei within lumens. The immature mesenchyme and epithelium mimic the embryonic lung at 10–16 weeks gestation. The name WDFA is therefore derived from the histological appearances of the tumor.6,7 Most are low grade with a favorable outcome. When mixtures occur with other histological subtypes, the tumor should be classified according to the predominant component.
A correct pre-operative diagnosis of endobronchial biopsies is difficult. Although a correct diagnosis may be achieved after resection, thorough sampling is essential, because the tumor may be heterogenic, with components characteristic of WDFA and pulmonary blastoma8 or components of more conventional adenocarcinoma. In both cases the prognosis is worse. Indeed, the 10-year survival for WDFA is about 75% versus about 15% for pulmonary blastoma. In our case the presence of this latter was excluded by conventional microscopy.
The standard treatment is surgical resection, if technically possible.
ConclusionThis case of well-differentiated fetal adenocarcinoma illustrates the importance of establishing an accurate diagnosis when a pregnant woman presents with respiratory symptoms by carrying out the necessary tests, obviously taking great care, especially when the symptomatic treatment does not provide any improvement. However, report emphasizes how important it is for clinicians to consider and identify this rare variant of adenocarcinoma because of its low grade malignancy associated with good prognosis.