Amyotrophic lateral sclerosis (ALS) is a fatal, progressive, neurodegenerative disease and most patients affected die of respiratory compromise and/or pneumonia within 2–3 years of diagnosis. As ALS progresses, ventilator assistance is required. In the end stages of the disease, patients suffer from respiratory failure and may become ventilator-dependent. Deaths due to malfunction of mechanical ventilators are reported but there are very few forensic autopsy records. We report the case of a 69-year-old ALS female ventilator-dependent, trachostomised patient who was found dead by her husband, with the ventilator in “stand-by” mode.
MethodA forensic autopsy was performed. Samples of internal organs were taken for histological and toxicological examination. The ventilator internal memory was also analysed and tested in order to find possible malfunction.
ResultsGross examination did not reveal any sign of trauma but showed brain and lung congestion. Pulmonary histological examination revealed thickening of peribronchial interstitial space, alveolar over-distension, break of inter-alveolar walls and diffuse alveolar haemorrhages. Focal microhemorrhages were also detected in other organs. Analysis of the ventilator internal memory showed that during the night of death, there had been several voltage drops. Specific tests revealed malfunction of the internal battery which was unable to provide the necessary voltage, as a consequence the ventilator switched off, stopping ventilation. Battery malfunction reduced the volume of the ventilator alarm, which was not heard by the caregiver.
ConclusionHistological pattern, with acute pulmonary emphysema and focal polivisceral haemorrhages, is strongly suggestive of a death due to “acute” asphyxia. The authors also discuss the need for strict supervision and follow up of these ventilatory dependent patients and their devices.
A Esclerose Lateral Amiotrófica (ELA) é uma doença fatal, progressiva e neurodegenerativa e a maioria dos doentes afectados morrerão de falha respiratória e/ou pneumonia 2 ou 3 anos após o diagnóstico. À medida que a ELA progride torna-se necessária a assistência ventilatória. Nos estágios finais da doença, os doentes sofrem de insuficiência respiratória e podem tornar-se dependentes do ventilador. São conhecidas mortes devido ao mau funcionamento de ventiladores mecânicos mas existem poucos registos forenses de tal situação. Relatamos o caso de uma doente de 69 anos com ELA, traqueostomizada e dependente do ventilador, que foi encontrada morta pelo seu marido com o ventilador em modo de espera («stand-by»).
MétodoFoi realizada uma autópsia forense. Foram recolhidas amostras dos órgãos internos para exame toxicológico e histológico. A memória interna do ventilador foi também analisada e testada de modo a descobrir uma possível avaria.
ResultadosO exame macroscópico não revelou qualquer sinal de trauma mas indicou congestão cerebral e pulmonar. O exame pulmonar histológico revelou o espessamento do espaço intersticial peribrônquico, sobredistensão alveolar, quebra de paredes interalveolares e hemorragias alveolares difusas. Foram detetadas micro-hemorragias focais noutros órgãos. A análise da memória interna do ventilador mostrou que, durante a noite da morte, houve diversas quedas de tensão. Testes específicos revelaram o mau funcionamento da bateria interna que não conseguiu fornecer a tensão necessária, consequentemente o ventilador desligou-se, parando a ventilação. O mau funcionamento da bateria reduziu o volume do alarme do ventilador, que não foi ouvido pelo prestador de cuidados.
ConclusãoO padrão histológico, com enfisema pulmonar agudo e hemorragias focais poliviscerais, é fortemente indicador de morte devido a asfixia «aguda». Os autores discutem também a necessidade de uma supervisão rigorosa e seguimento destes doentes dependentes do ventilador e dos seus equipamentos.
Amyotrophic lateral sclerosis (ALS) is a devastating disease involving both upper and lower motor neurons. It is the most common form of motor neuron disease, affecting approximately 1.2 to 1.8/100,000 individuals. Clinically, ALS is characterised by progressive muscular weakness leading to loss of the ability to move and speak and, in almost all patients, causes death between 3 and 5 years from diagnosis. Cortical and cognitive functions remain essentially unchanged.1
Respiratory failure is the most common cause of morbidity and mortality in these patients. Reduction in respiratory muscle strength with ineffective alveolar ventilation and difficult airway secretions clearance may lead to chronic respiratory insufficiency (CRI) and potentially life-threatening problems. Long term mechanical ventilation (LTMV) delivered either invasively or non invasively is the main therapeutic intervention to support the respiratory muscle function and to increase life expectancy and health-related quality of life (QOL).2
Literature evaluating survival of ALS patients receiving LTMV via tracheostomy is scarce and contains conflicting reports, with considerable variation among studies as to the time between starting this treatment and death.3 Quality control of the equipment used and risk management are important aspects of LTMV in order to ensure that patients receive the prescribed ventilatory support safely and accurately.4,5 Deaths due to malfunction of mechanical ventilators are reported but forensic autopsy records are rare.6 We report the case of a 69-year-old trachostomised, ventilator-dependent ALS female patient, found dead by her husband.
Case reportA 69-year-old female had been diagnosed as having had ALS for 2 years. She had been 24/24h ventilator-dependent, under tracheostomy LTMV for 18 month after a previous 9-month period of mask ventilation. Lung function test at initiation of NIV showed mild restriction (slow vital capacity (SVC): 61% pred, forced expiratory volume at 1s (FEV1): 60% pred, FEV1/SVC:99%). Tracheostomy had been electively performed after progressive worsening of gas exchanges (PaCO2 59mmHg) symptoms and lack of compliance to NIV. In fact, the patient had not tolerated NIV for more than 2h per night. She was also on enteral nutrition (EN) through percutaneous gastrostomy (PEG). In the last 12 months the patients underwent two admissions to the emergency department for non-respiratory causes, and had no major problem in the last four months before she was found dead in her bed by her husband. No resuscitation maneuver was performed.
The night before, her husband had checked ventilator and EN pump and had found nothing unusual. Early in the morning he was woken up by the alarm of the EN pump: he realized that his wife was not breathing and pulseless. The ventilator was in “stand- by” mode.
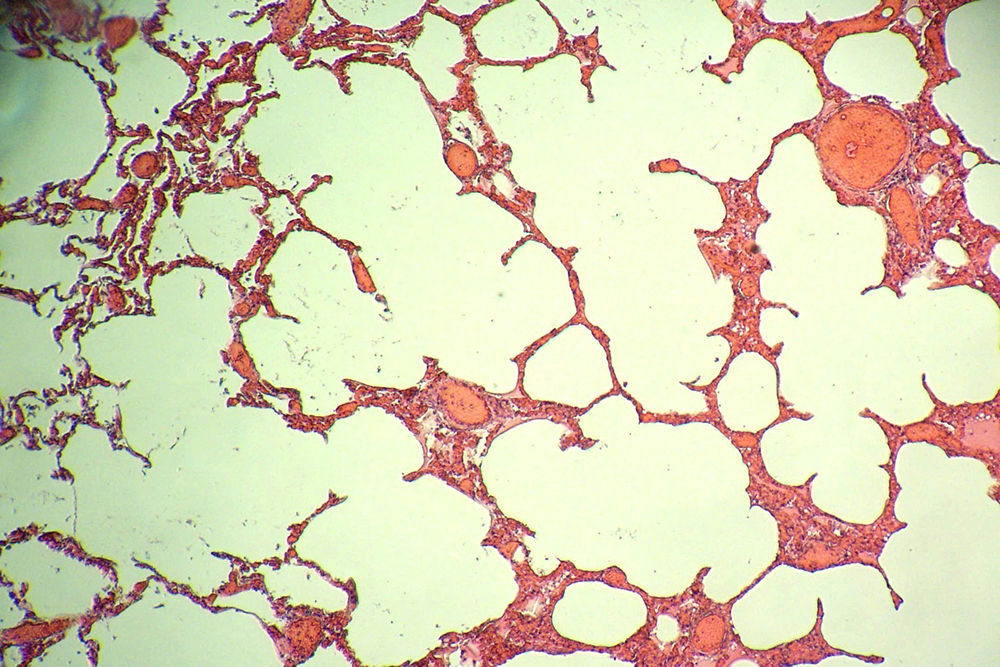
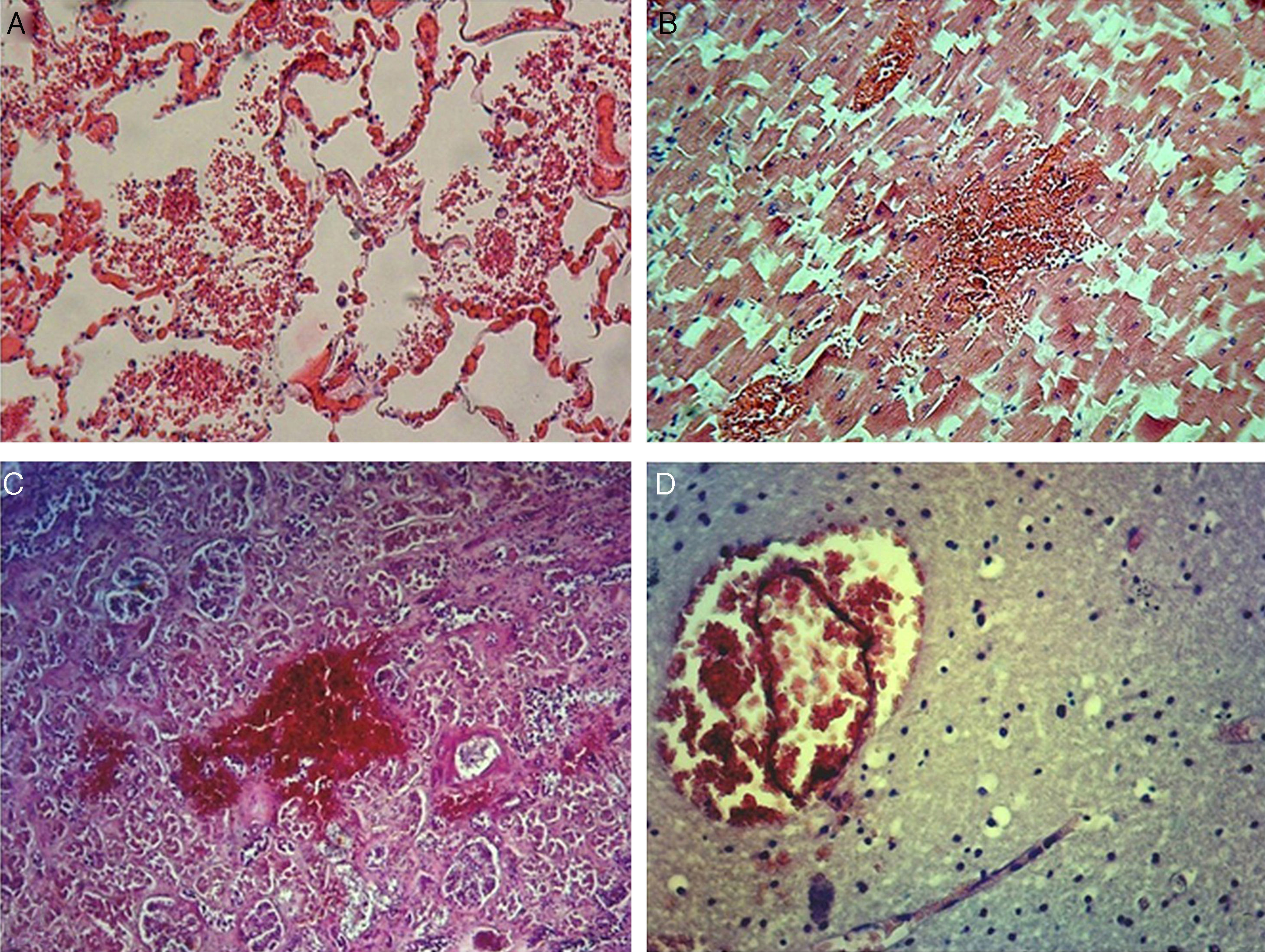
At autopsy, gross examination did not reveal any trauma sign but showed brain oedema and congestion and lung congestion. Pulmonary histological examination revealed a slightly thickening of peribronchial interstitial space, alveolar overdistension with alveolar rupture and diffuse alveolar haemorrhage, alveolar capillary congestion (Fig. 1). Focal microhemorrhages were detected also in lungs, kidneys, liver, heart, brain and adrenal glands tissue (Fig. 2). Oxicological examination was negative.
Analysis of the internal memory of the ventilator, showed that during the night, several voltage drops had happened. Specific technical tests revealed malfunction of the ventilator internal battery, unable to provide the necessary voltage had caused the ventilator stop. Battery malfunction also reduced the alarm volume which was not heard by caregiver.
DiscussionRespiratory failure is the most common cause of death in ALS patients. In this case, cause of death was attributed to ventilator pump failure related to acute asphyxia. Asphyxia is a broad term including a variety of conditions resulting in interference with oxygen uptake or utilization,7 particularly in the brain. In the forensic context, death typically results from mechanically induced cerebral hypoxia.
All ventilators provided with an expiratory valve allow the patient to breath in room air in case of ventilator malfunctioning. The valve always remains open when the ventilator stops. Only a severe valve malfunctioning can explain asphyxia in a patient still actively breathing. However the likelihood of this valve malfunctioning is very low because in case of valve membrane rupture (so called mushroom valve) the valve leaks still allow the patients to breath in room air. But in this case it is not likely that our 24/24 hour ventilatory-dependent patient would still have the residual strength for breathing activity and this would explain the acute asphyxia.
Pulmonary histological examination revealed thickening of peribronchial interstitial space, alveolar over-distension, break of inter-alveolar walls and diffuse alveolar haemorrhages that can also go along with the hypothesis of barotraumas in a long term ventilated patient. In the present case histological pattern showed high grade of acute pulmonary emphysema allowing us to hypothesize long-term barotrauma effect.
Ventilator-dependent patient management, including periodic check and maintenance of the ventilator, is crucial. A survey covering 16 European countries showed that: (1) ventilator servicing was mainly carried out by external companies, with a servicing frequency ranging 3–12 months; (2) interaction between servicing companies and prescribers was limited; (3) participation of centres in equipment quality control was poor; and (4) centres were insufficiently aware of vigilance systems.4 Chatwin et al.5 examined the nature of calls to a home support helpline to identify patient/equipment problems and strategies to minimise risk for patients, healthcare teams and manufacturers. From adult and paediatric patients with neuromuscular disease, chronic obstructive pulmonary disease or chest wall disease receiving LTMV, and all calls to a dedicated respiratory support telephone hotline in a six-month period were analysed. Out of 1211 patients 1119 received non-invasive ventilation, 12 tracheostomy ventilation; 149 had two ventilators for 24-h ventilator dependency. There was a mean of 528 daytime calls per month and 14 calls a month at night. Following 188 calls, a home visit was performed; these identified a technical problem that could either be solved in the patient's home in 64% or required replacement or new parts in 22% of cases. In 25 calls in which no mechanical fault was identified, 13 patients were either found to be unwell or required hospital admission. Authors conclude that patients using LTMV have a substantial need for assistance, with most technical problems being resolved simply. Where no fault was found during an equipment check, the patient themselves may be unwell and should receive early clinical evaluation. The patient may have mistaken clinical deterioration for an equipment problem.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.