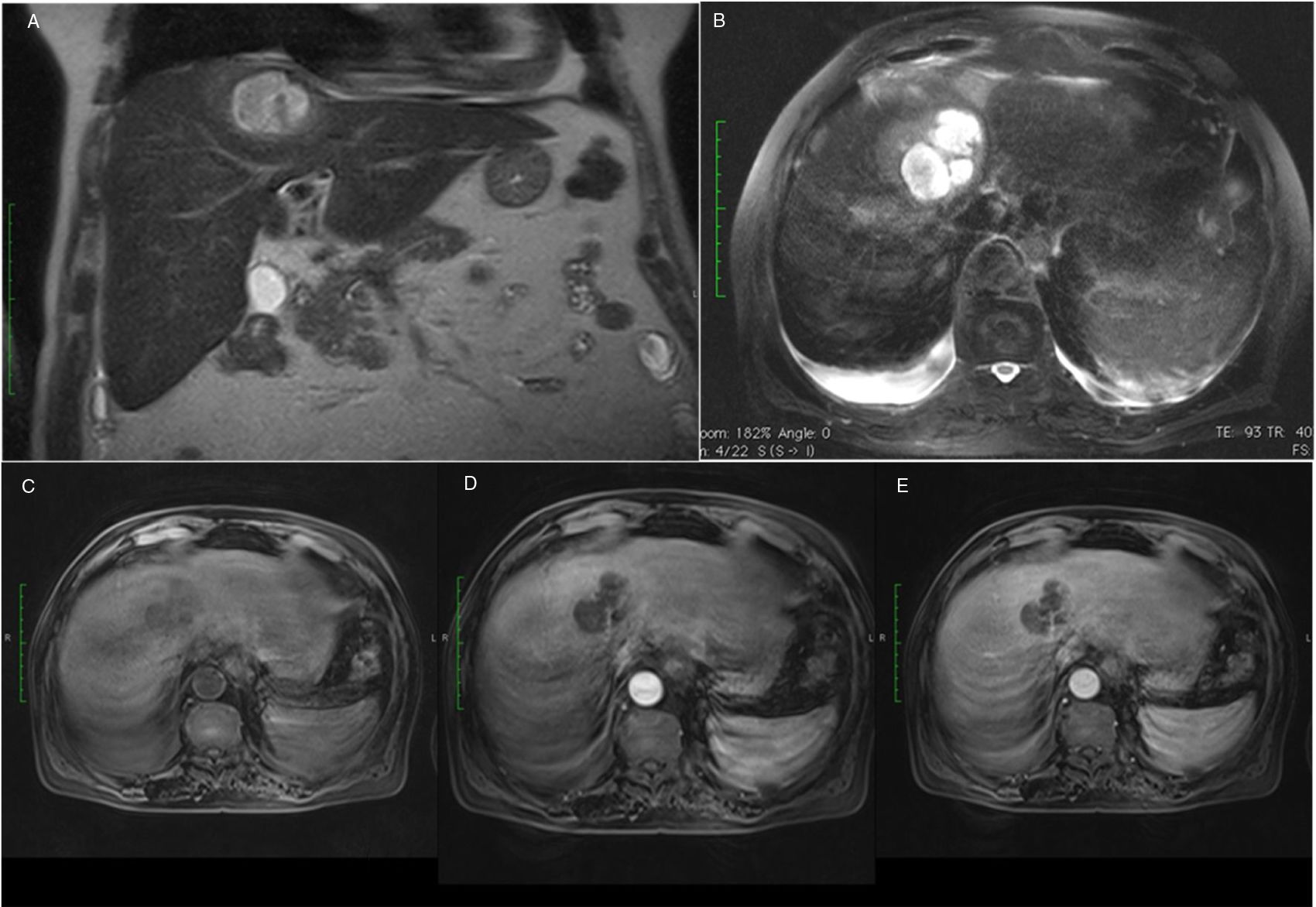
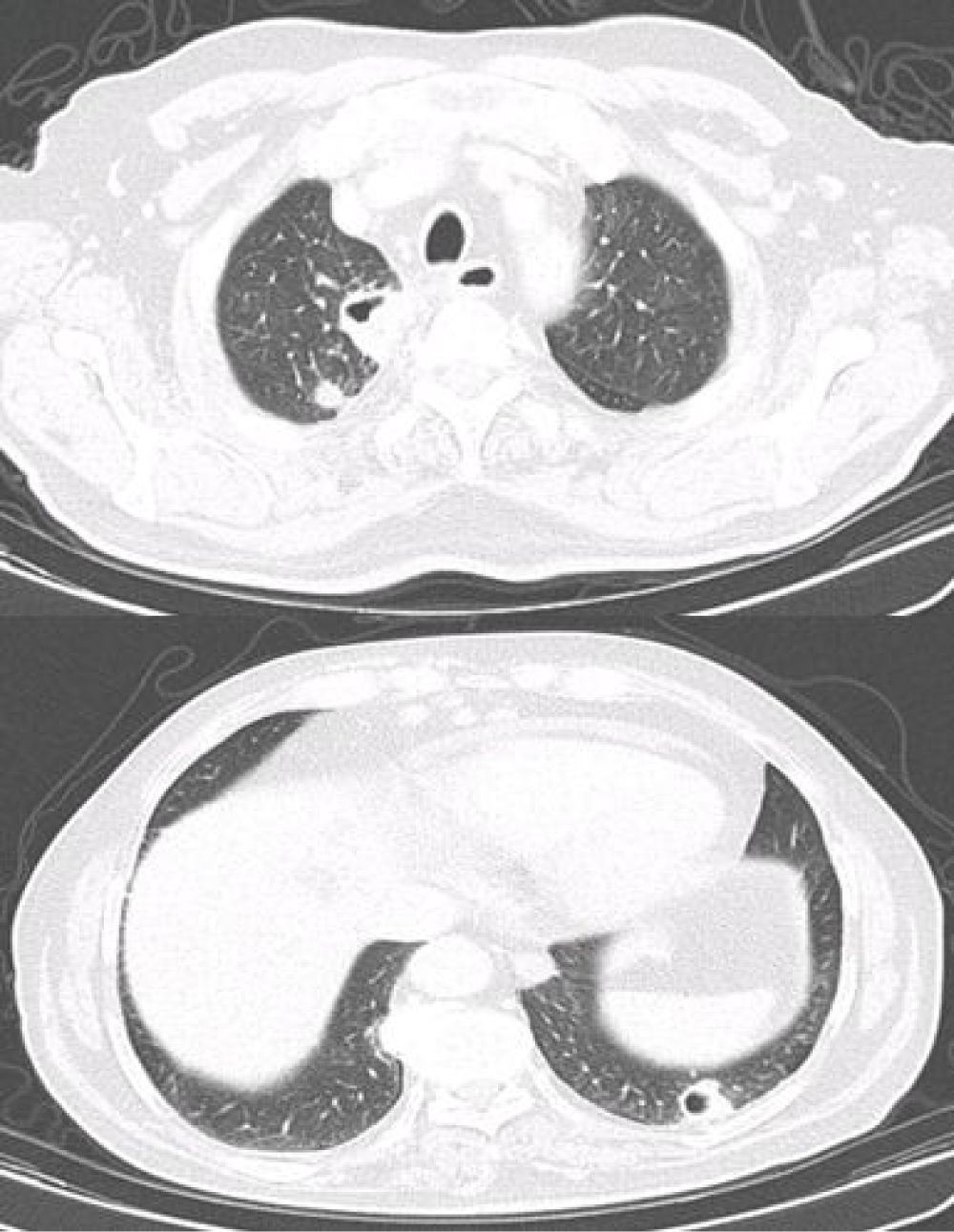
A 74-year-old caucasian male, presented with a two-week history of fever, shivering, right scapular pain and dry cough. His medical history recorded high blood pressure, smoking and alcohol drinking. He had no recent history of antibiotic use, hospitalization or travelling to foreign countries. On admission he was sweaty and febrile, without any other significant alterations on physical examination. Laboratory analyses detected hypocapnia, elevated white blood count, C-reactive protein level as well as elevated liver enzymes. Chest X-ray revealed faded round densities on both lungs while abdominal ultrasound showed an hyperreflective liver with an oval, hypoechoic and heterogenic lesion (7.3 × 3.9 cm). Patient was hospitalized and started on doxicicline. Abominal MRI confirmed the nodular lesion in the the IV/VIII segments of the liver, with fluid and internal septae (Fig. 1). Simultaneously, the patient was diagnosed with diabetes mellitus and Kp resistant only to ampicillin was isolated in 2 blood cultures. The antibiotic was changed to amoxicillin-clavulanic acid plus metronidazole and the patient became afebrile and without pain. Percutaneous drainage was not executed due to high risk related to subphrenic location. Subsequent contrast CT-scan also revealed multiple nodules on both lungs, mostly peripheral, the bigger ones being cavitated and were considered as septic pulmonary emboli (Fig. 2). The patient was discharged after 2 weeks, antibiotics were continued until 8 weeks and no recurrence has been reported after 2 years .
Abdominal MRI (A) Coronal plan, T2 HASTE sequences – nodular lesion in the IV/VIII segments of the liver (B) Axial plan, T2 FS weighted sequences – hypersignal with fluid and internal septae (C) before gadolinium injection (non-enhancement phase) (D) after gadolinium injection, arterial phase – without contrast enhancement (E) after gadolinium injection, portal phase- peripheral contrast enhancement of the lesion.
We believe that this patient had a distinctive form of community acquired Klebsiella pneumoniae (Kp) infection causing liver abscess and complicated with septic metastatic pulmonary emboli, forming abscesses.
Liver abscess due to Klebsiella pneumoniae (KLA) is a distinct syndrome characterized by monomicrobial liver abscess, almost exclusively acquired in the community and in the absence of hepatobiliary disease. It is strongly associated with diabetes mellitus and Asian ethnicity and has a higher probability of complicating with metastatic infection sites than liver abscesses of other etiologies.2 Some particularly virulent strains expressing hypermucoviscous phenotype are responsible for this invasive syndrome, despite not being naturally resistant to antibiotics.3 It was geographically confined to Southeast Asia until the past decade, when other reported cases indicate the emergence of this syndrome worldwide.3 In up to 11–12% of cases, KLA can be complicated with other septic metastatic lesions.3
Our patient was Caucasian and a 74-year-old male, consistent with published demographic data.3 He fulfilled the requested diagnosis criteria for KLA2,5,6; 1. Clinical symptoms and laboratory findings of liver abscess: fever, chills, referred scapular pain, elevation of white-blood cell count and C-reactive protein, abnormal liver function tests; 2. Compatible imaging: as in this case, KLA has distinctive imaging features, being more often single, solid in appearance and septated, comprising multiple non-communicating locules; 3. Isolation of Kp in blood culture/abscess aspiration culture: although serotyping was not conducted, antimicrobial susceptibility of Kp isolated in blood culture meets the characteristic pattern of virulent KLA, described to be resistant to ampicillin and ticarcillin/carbenicillin but susceptible to all other antibiotics.2,3,5
That this patient had no underlying hepatobiliary disease, no previous hospitalizations or antibiotic use having acquired Kp in the community, also favored this diagnosis. Furthermore, he was simultaneously diagnosed with diabetes mellitus, the most common host risk factor for KLA.3 Metastatic complications are more frequent in KLA than liver abscesses of other etiologies2; They can occur in up to 11–12%, most commonly as endoftalmitis and meningites but SPE is a rare complication and it is generally present at hospital admission.3–6 Our patient met SPE diagnostic criteria: had dry cough and hypocapnia, lung infiltrates, KLA as the embolic source, other potential explanations for lung infiltrates excluded and lung infiltrates resolved after appropriate antimicrobial therapy.5,6 A broad spectrum of CT-scan findings can be present but less commonly compatible with lung abscesses.6
In conclusion, we describe a case of KLA with high clinical importance since it is the second case reported in Portugal 1, and the only one with the exceptionally rare complication of lung abscesses.3,4,7 This case is an additional proof of the emergence of this syndrome worldwide. In cases of multiple lung abscesses with an acute presentation with dry cough in diabetic patients Kp should be considered, since it may be the first manifestation of serious underlying infection.