The mediastinum is an anatomic compartment in the thoracic cavity located between both pleural cavities.1 Pneumomediastinum is a rare clinical condition in which air leaks into the mediastinum2,3 resulting from physical trauma or other situations that lead to air escaping from the lungs, airways or bowel into chest cavity.
It has an incidence of 1: 44,500 patients admitted to the emergency room3 and it may also be spontaneous4 or secondary to other clinical situations (iatrogenic or non-traumatic).2,3 The majority of patients are males accounting for 76% of reported cases. Many authors believe that it is an underdiagnosed condition as symptoms may be easily attributed to other causes.3 One of the possible etiologies is an abnormal increase of intra-mediastinal pressures,3 which forces the air into the intra-thoracic tissues to balance pressures.5,6
Diving associated pneumomediastinum has been progressively increasing and occurs mainly during the decompression phase.7 Patients may have cervical pain or swelling,2 dyspnea, cough, thoracalgia2,6 and less frequently anxiety, dysphagia, sialorrhea and fever.2
Although the diagnosis is usually confirmed by thoracic radiography,3 this exam may be normal in about 30% of the patients2 and for these, a computed scan tomography (CT) is mandatory.3 Laboratory findings are frequently inconclusive but some may reveal minor elevation of inflammatory parameters.3
The authors present the case of a 21-year-old male professional fisherman, who, after 90 min of surface diving, increased dive depth to seven meters with compressed air bottle. At this point he emerged rapidly after feeling an unusual thoracic discomfort, which become worse as he ascended. Immediately after the emersion he developed complaints of cervical swelling and dysphonia, and was admitted to our hospital emergency department. Physical examination revealed a subcutaneous cervical and supraclavicular emphysema in chest radiography (Fig. 1), which later extended to the abdominal region. The patient remained hemodynamically stable, with peripheral oximetry between 98 and 100% breathing room air.
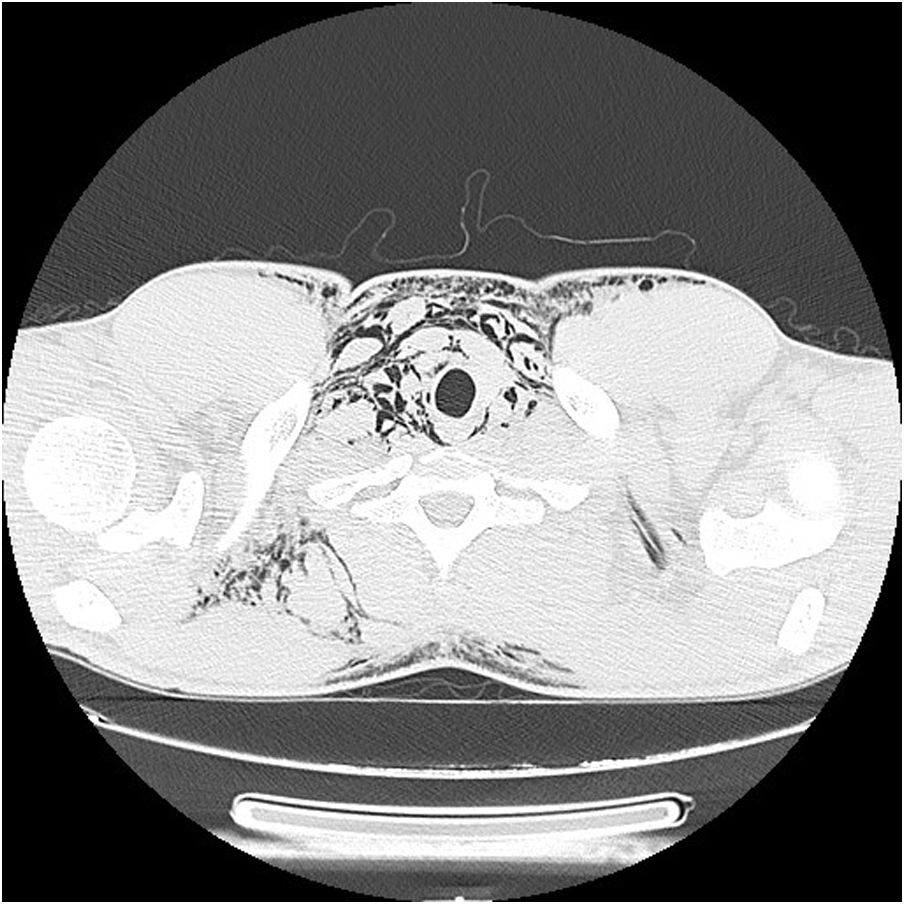
Besides a smoking habit (seven smoking pack year) his previous medical history was unremarkable. No relevant alterations in peripheral blood analysis were observed but thoracic CT confirmed the presence of pneumomediastinum with subcutaneous emphysema (Fig. 2). The Hyperbaric Medicine Service decided that the patient did not need be exposed to hyperbaric treatment as there were no neurological symptoms. Nasal canula oxygen treatment was initiated to increase gas reabsorption and he was closely monitored for potential esophagic or tracheal rupture in the following 24 h.
After that period, patient was discharged as there was total subcutaneous and mediastinal emphysema reabsorption without evident sequelae. The subsequent follow-up appointment showed no clinical or imagiological evidence of relapses. He followed a respiratory functional study as an outpatient which was normal.
Pneumomediastinum is usually a benign medical situation3 and although there is no consensus regarding treatment, most studies support a conservative approach with rest and analgesia.6 Oxygen administration can increase gas reabsorption up to six-times and should be considered as an alternative treatment.3 Relapses are rare, so a short-term medical surveillance is recommended.3 This condition may be responsible for a high incidence of morbimortality such as facial or cervical lesions and esophagic or tracheal rupture,2 which justifies a complementary study carried out after the acute onset. Although spirometry is not recommended in the acute setting, however, it must be performed to exclude pulmonary fragility that may worsen the overall pneumomediastinum prognosis.
With this case, the authors aim to alert to a rare and otherwise underdiagnosed situation which, although benign, requires a prompt diagnosis and acknowledgement of the risks that may be associated.
FundingThe authors declare that no funding was received for this paper.
Conflicts of interestThe authors have no conflicts of interest to declare.
Author contributions- -
Catarina Cascais-Costa wrote the paper.
- -
Gilberto Teixeira contributed to data collection.
- -
Gilberto Teixeira and Lília Andrade contributed to the revision of the manuscript.
- -
All the authors read and approved the final manuscript.