Until recently, cystic fibrosis (CF) was considered a paediatric disease, and transition of patients to adult care was rarely performed due to low life expectancy and reduced experience from adult Medicine in the follow-up of this disease. Nowadays, due to significant improvement of CF survival rates, almost all of these patients reach adulthood.1,2 The transference of teenagers with a chronic disease like CF to adult care is a very stressful phase, sometimes faced with some anxiety by both parents and patients. Therefore, a transition period is fundamental for both, with the aim of promoting the patient's autonomy and acceptance of new roles, but also giving continuity of care. In the Specialized Centre of Cystic Fibrosis (SCCF) of the Hospital Santa Maria (Lisbon), this transition happens over three appointments, where both paediatric and adult physicians are present. Since the implementation of this programme in 2000, 54 young adults have been transferred to adult care.
The aim of this study was to characterize the clinical status of CF patients during the year of transition to adult care in a 7-year period.
We conducted a retrospective, descriptive study of all patients transferred to adult care between January 2010 and December 2016. Clinical records were reviewed and the following data were obtained: sex, age at diagnosis, genotype, treatment performed, complications, airway bacterial colonization, lung function (forced expiratory volume in 1s (FEV1)) and nutritional status (body mass index – BMI) in the year of transition. IBM SPSS v21.0® and Microsoft Excel 2013® were used for the descriptive analysis.
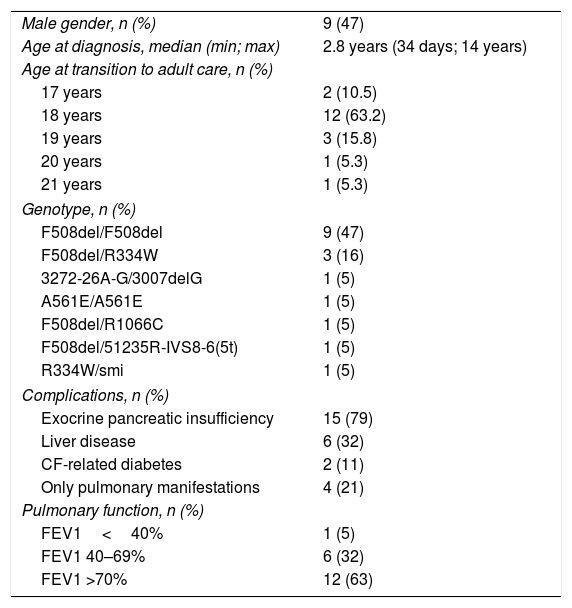
From a total of 87 patients followed at the SCCF during the study period, 25 had reached adult age, of which 19 were transferred to adult Pulmonology. The main reasons for delay in transfer to adult care were either clinical instability or personal reasons (e.g. waiting for placement in University in another city). Nine (47%) patients were male, median age at diagnosis was 2.8 years [minimum 34 days; maximum 14 years] and 9 were homozygous for F508del mutation. Most patients (79%, n=15) presented exocrine pancreatic insufficiency, six (32%) had liver disease, two (11%) CF-related diabetes and four (21%) had only pulmonary manifestations (Table 1). All patients were transferred to adult care up to the age of 21 years, the majority (63%, n=12) at 18 years.
Sample characterization (n=19). CF=cystic fibrosis.
| Male gender, n (%) | 9 (47) |
| Age at diagnosis, median (min; max) | 2.8 years (34 days; 14 years) |
| Age at transition to adult care, n (%) | |
| 17 years | 2 (10.5) |
| 18 years | 12 (63.2) |
| 19 years | 3 (15.8) |
| 20 years | 1 (5.3) |
| 21 years | 1 (5.3) |
| Genotype, n (%) | |
| F508del/F508del | 9 (47) |
| F508del/R334W | 3 (16) |
| 3272-26A-G/3007delG | 1 (5) |
| A561E/A561E | 1 (5) |
| F508del/R1066C | 1 (5) |
| F508del/51235R-IVS8-6(5t) | 1 (5) |
| R334W/smi | 1 (5) |
| Complications, n (%) | |
| Exocrine pancreatic insufficiency | 15 (79) |
| Liver disease | 6 (32) |
| CF-related diabetes | 2 (11) |
| Only pulmonary manifestations | 4 (21) |
| Pulmonary function, n (%) | |
| FEV1<40% | 1 (5) |
| FEV1 40–69% | 6 (32) |
| FEV1 >70% | 12 (63) |
Regarding pulmonary function, six (32%) patients presented FEV1<70%, of which only 1 had severe obstruction (FEV1<40%) (Table 1).
Concerning nutritional status, three patients (16%) had a BMI<18kg/m2.
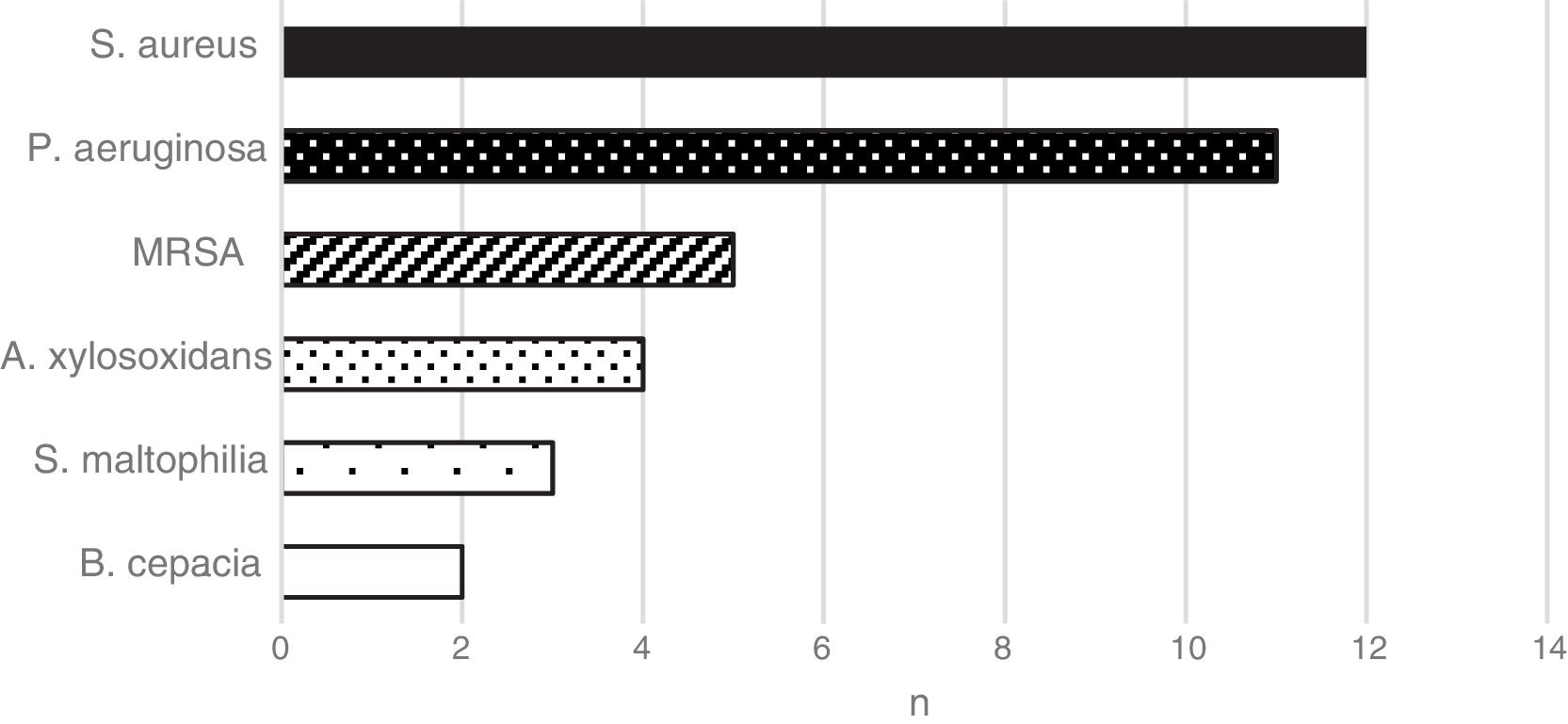
As for airway bacterial colonization, the most common microorganisms isolated during the year of transition were Staphylococcus aureus (n=12) and Pseudomonas aeruginosa (n=11) (Fig. 1), which were responsible for chronic colonization in 57.9% and 31.6% of patients, respectively.
In terms of treatment, 13 (68%) patients had inhaled antibiotics, 16 (84%) dornase alfa and 16 (84%) pancreatic enzymes. No patients were on home oxygen therapy.
With improvements in healthcare in the last decades, nowadays 85% of chronic paediatric patients reach adulthood,3 highlighting the importance of continued care and transition programmes to adult Medicine. Understanding the clinical condition in which patients reach adulthood is of utmost importance, as an audit of paediatric clinical care and for future comparison of outcomes.
In CF patients, not only has life expectancy increased, but nutritional status and quality of life have also improved, which are known to correlate to better respiratory function.6
To our knowledge, this is the first study published in Portugal to describe this reality.
We hope these results can be used for future comparison and evaluation of outcome improvements in CF patients, namely the ones who were lately diagnosed through the neonatal screening programme, most of which began follow-up and treatment even before onset of symptoms. We hypothesize that they will have better nutritional status and pulmonary function at transition to adult care, as has been previously reported.4–6
Conflicts of interestThe authors have no conflicts of interest to declare.