Asthma and COPD are respiratory diseases in which a better knowledge and understanding of the pathology allows the patients to be more involved, which is crucial in their treatment. Holding educational sessions is a good way of imparting information to the patients.
AimTo determine the efficacy of educational sessions in helping patients with asthma and COPD to acquire a better understanding of their condition.
MethodsFollowing a Portuguese Lung Foundation initiative to improve knowledge about respiratory health, educational sessions for patients suffering from asthma or COPD were organized. 25 randomized patients with each disease were invited to participate. Each session lasted 60min. Patient knowledge was tested by means of a multiple choice questionnaire before and after the session.
ResultsFifteen patients with asthma attended the sessions; they had an average age of 36 years, of which 60% were female. Within the group 60% were able to name their pathology correctly. Seventeen patients with COPD attended the sessions; they had an average age of 69 years, of which 70% were males and only 3 (17.6%) patients were able to correctly name their pathology. In both groups, there was a statistically positive improvement (p<0.05) of correct answers to the questionnaire at the end of each educational session.
ConclusionPatient knowledge increased in each educational session. Patients with COPD were less well informed about their disease than patients with asthma and they also had more difficulty in correctly naming their disease.
Asma e DPOC são patologias respiratórias em que o envolvimento e conhecimento dos doentes é determinante no tratamento. Uma forma de esclarecimento e informação é a realização de sessões de educação para doentes.
ObjetivoAvaliar a eficácia de sessões de educação para doentes com Asma e DPOC na aquisição de conhecimentos.
MétodosA propósito da uma iniciativa da Fundação Portuguesa do Pulmão, com o intuito de promover o conhecimento sobre a saúde respiratória, foram realizadas sessões de educação para doentes com diagnóstico de Asma e DPOC.
Foram selecionados aleatoriamente 25 doentes cada um dos diagnósticos referidos e convidados a participar. Cada sessão teve a duração de 60minutos. O conhecimento foi avaliado utilizando um questionário de escolha múltipla realizado antes e depois de cada sessão.
ResultadosParticiparam 15 doentes com asma, com média de idade de 36 anos, sendo 9 (60%) do sexo feminino; 60% dos doentes sabiam nomear corretamente a sua patologia. Dos doentes com DPOC participaram 17, com média de idade de 69 anos, 12 (70%) eram do sexo masculino e apenas 3 doentes nomearam corretamente a sua patologia respiratória. Em ambos os grupos verificou-se melhoria estatisticamente significativa (p<0,05), das respostas corretas ao questionário após cada sessão de educação.
ConclusãoVerificou-se um aumento de conhecimento dos doentes em ambas as sessões de educação. Os doentes com DPOC parecem ter menor informação sobre a sua doença e têm maior dificuldade em denominá-la.
Asthma and COPD are respiratory diseases with high incidence in the general population and a tendency to increase is forecasted.1,2 Both diseases are associated with high work and/or scholastic absenteeism3–6 and both have a strong impact on health expenses7,8; they are also associated with bad health habits which could be avoided, hence the efforts being made to control these diseases more effectively.1,2,7
Several studies have demonstrated that patient education reduces hospital admissions, the number of medical appointments and labor absenteeism and also improves quality of life.9–11 Other studies demonstrated that benefits in lung function12,13 and adherence to treatment14 are more obvious in asthma patients and that the cost/benefits confirm the advantage of educating both patients with asthma and COPD.10,11
Patient education is currently recommended in several clinical guidelines.1,2,15 Diverse forms of patient education are presented in different studies9–14 but given the consistency of the results we may consider “access to information” as the determining factor. There is considerable variation in the number, regularity and type of educational sessions, number of participants (individual/group) and the characteristics of the educators (doctors/nurses).
In the present study the authors aim to evaluate the efficacy of a 60-min educational session given by a pulmonologist for patients with asthma and COPD, by measuring the variation in correct answers given before and after each session to a questionnaire.
MethodsThe “Semana do Pulmão” initiative was organized by the Portuguese Lung Foundation to improve respiratory health knowledge in the population in general and for those suffering from respiratory pathologies in particular. There were subsequently a number of initiatives in partnership with the Unidade de Saúde Familiar Nova Via (ACES Espinho/Gaia) in the North of Portugal in October 2010.
Twenty-five randomized patients with each of above mentioned diseases were selected from the health care unit database and invited to participate in educational sessions. The patients had been diagnosed and followed by their General Practitioners, according to clinical guidelines.1,2
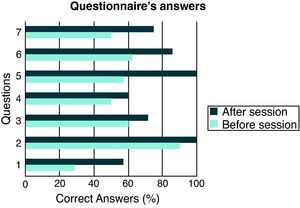
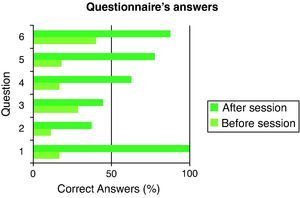
There was an educational session for asthma patients and another for COPD patients. Each session lasted 60min. Before and after attending a session, each patient completed an electronic anonymous multiple choice questionnaire with 4 or 5 options and 60s time limit per question (Fig. 1) and a demographic questionnaire.
Visual support was used in both educational sessions, and definition, prevalence, risk factors, clinical characteristics and treatment were briefly described. Afterwards, there was a demonstration of inhalation techniques using several devices; at this point the patients were invited to ask questions and clarify any remaining doubts.
The demographic characteristics, smoking habits, severity of disease and the length of time since diagnosis were evaluated for each patient. The patients’ ability to correctly name their own disease was also analyzed.
Statistical analysis of the pre- and post-session questionnaires was conducted using SPSS 18 for a demographic evaluation of the patients and using the Wilcoxon test for statistical significance assessment.
ResultsFrom the 25 selected patients to take part in each session, 15 participated in the asthma session and 17 in the COPD session.
In the asthma educational session the average age of the participants was 36 years (6–72 years); 9 patients were female (60%) and 6 were male. Four patients were smokers, 2 ex-smokers and 9 non-smokers. The median time gap between the diagnosis and the educational session was 10.3 (40–1) years. According to GINA classification of asthma severity,1 the majority of the patients had mild persistent asthma (61.5%) and intermittent asthma (30.8%). Only 8 patients declared their educational level, 2 had college degrees, 3 had high school level education and the remaining had only primary education (4 years).
When asked the name of the respiratory disease affecting them 9 patients (60%) answered “asthma”, 3 (20%) answered “bronchitis” and 3 (20%) could not answer (Table 1).
Patient characteristics.
| Characteristics | Asthma | COPD |
| Mean age (years) | 36 (6–72) | 69 (53–82) |
| Sex | ♂ 6 (40%) | ♂ 12 (70%) |
| ♀ 9 (60%) | ♀ 5 (30%) | |
| Smoking habits | ||
| Smoker | 4 (26.7%) | 5 (29.4%) |
| Ex-smoker | 2 (13.3%) | 6 (35.3%) |
| Non-smokers | 9 (60%) | 6 (35.3%) |
| Mean time between the diagnosis and the questionnaire | 10.3 (40–1) | 2.8 (6–0.5) |
| Disease severity | Intermittent – 30.8% | Stage I – 18.2% |
| Mild persistent – 61.5% | Stage II – 72.7% | |
| Moderate persistent – 7.7% | Stage III – 9.1% | |
| Ability to name correctly their pathology | Yes 9 (60%) | Yes 3 (17.6%) |
| No 6 (40%) | No 14 (82.4%) | |
The questionnaire consisted of 7 questions; the average of initial correct answers was 57% (28.5–90%) and that of the final correct answers was 78% (57.10–100%). There was a statistically significant (p=0.02) improvement in the answers of the patients (Fig. 2).
In the COPD educational session the average age of the patients was 69 years (53–82 years); 12 patients were male (70%) and 5 female. Five patients were smokers, 6 ex-smokers and 6 non-smokers. The median time gap between the diagnosis and the educational session was 2.8 (6–0.5) years. According to GOLD classification of disease severity,2 the majority of the patients had stage II COPD (72.7%). Only 2 patients declared their education level and both had only primary education (4 years).
When asked the name of their respiratory disease, 3 patients (17.6%) answered “COPD”, remarkably 8 patients answered “bronchitis” (47.1%) and 1 (5.9%) answered “emphysema” (Table 1).
The questionnaire used had 6 questions and the average of initial correct answers was 21.9% (11–40%) and that of final correct answers was 68.3% (37.5–100%). There was a statistically significant (p=0.03) improvement in the answers of the patients (Fig. 3).
DiscussionThe importance and benefits of educating patients with asthma and COPD is widely accepted.10,11 In these diseases the low compliance, the inability to recognize individual triggers, the impact of risk factors and their avoidance are associated with the inability to control the disease and deaths that could be avoided.2,7,16 Educational sessions that allow patients to recognize the crucial role they have in controlling their own disease led to improved adherence rates and consequent disease control.9–15
This study is limited by the small sample size and single geographic location, and so does not allow result extrapolation to other wider groups such as the Portuguese population. The characteristics of the remaining individuals that had been selected but did not participate in the sessions were not considered. Since the questions with worse performance in the asthma educational session were in a negative format (wrong answer requested), comprehension of the questionnaire could be considered as a confounder in the performance evaluation. Additionally, the diagnoses of respiratory diseases, although performed in accordance to existing regulations, were not made by Specialists.
In relation to the analysis of the demographic data, according to what is described in the literature, there is a higher prevalence of males in the COPD patient group, while the asthma patients were younger. Against expectation, we noted a high prevalence of non-smokers in the COPD group, it may be that their disease is the result of occupational exposure. The average of initially correct answers was higher in the asthma group, which perhaps could be explained by the fact that there was a significantly longer time period between diagnosis and educational session compared to COPD patients and by the fact that the group asthmatic patients were younger, which would facilitate the cognition mechanisms. Although not a factor analyzed, it was found that the patients with asthma were more participative and asked more questions throughout the session. It may be that age and education level are factors that affect the access to and acquisition of information and interest displayed. Unfortunately only a small proportion of the patients gave their educational level so it was not possible to correctly analyze this parameter.
The answers obtained in the initial questionnaire suggest that the patients’ knowledge of their own respiratory diseases was limited. This may be due to the fact that for the majority of patients in both groups the severity of the disease was mild to moderate.
The variation of correct answers between pre- and post-session questionnaires showed statistically significant improved knowledge and the authors felt positive about the value of these sessions. These findings would not seem to be exclusive to respiratory patients; similar results have been obtained in several chronic diseases such as hypertension, Diabetes mellitus and obesity, where adherence to treatment and patient education is crucial.17–19
It is also interesting that only a small number of COPD patients use this terminology to describe their respiratory pathology. For many years, terms such as bronchitis and emphysema were used to describe this group of patients and maybe this kind of nomenclature is more comprehensible to the general population than an acronym.
If we accept that the acquisition of knowledge is crucial, sessions such as those presented in this study appear to be effective and useful. Nevertheless, we should consider that an effective education is a continuous process, so sessions like these should be part of a long term educational plan in order to consolidate patient knowledge and maximize benefits.
ConclusionThe educational sessions for patients with asthma and COPD diagnosis led to an improvement in the patients’ knowledge about their own pathology.
Patients with COPD seemed to know less about their disease than patients with asthma and had greater difficulty in correctly naming their pathology.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: van Zeller M. Avaliação de eficácia de sessões de educação a doentes com asma e DPOC. Rev Port Pneumol. 2012. doi:10.1016/j.rppneu.2011.07.005.