Helmet continuous positive airway pressure (CPAP) has been widely used during the COVID-19 pandemic. Specific filters (i.e. High Efficiency Particulate Air filter: HEPA; Heat & Moisture Exchanger Filter: HMEF) were used to prevent Sars-CoV2 environmental dispersion and were connected to the CPAP helmet. However, HEPA and HMEF filters may act as resistors to expiratory gas flow and increase the levels of pressure within the hood.
MethodsIn a bench-top study, we investigated the levels of airway pressure generated by different HEPA and HMEF filters connected to the CPAP helmet in the absence of a Positive End Expiratory Pressure (PEEP) valve and with two levels of PEEP (5 and 10 cmH2O). All steps were performed using 3 increasing levels of gas flow (60, 80, 100 L/min).
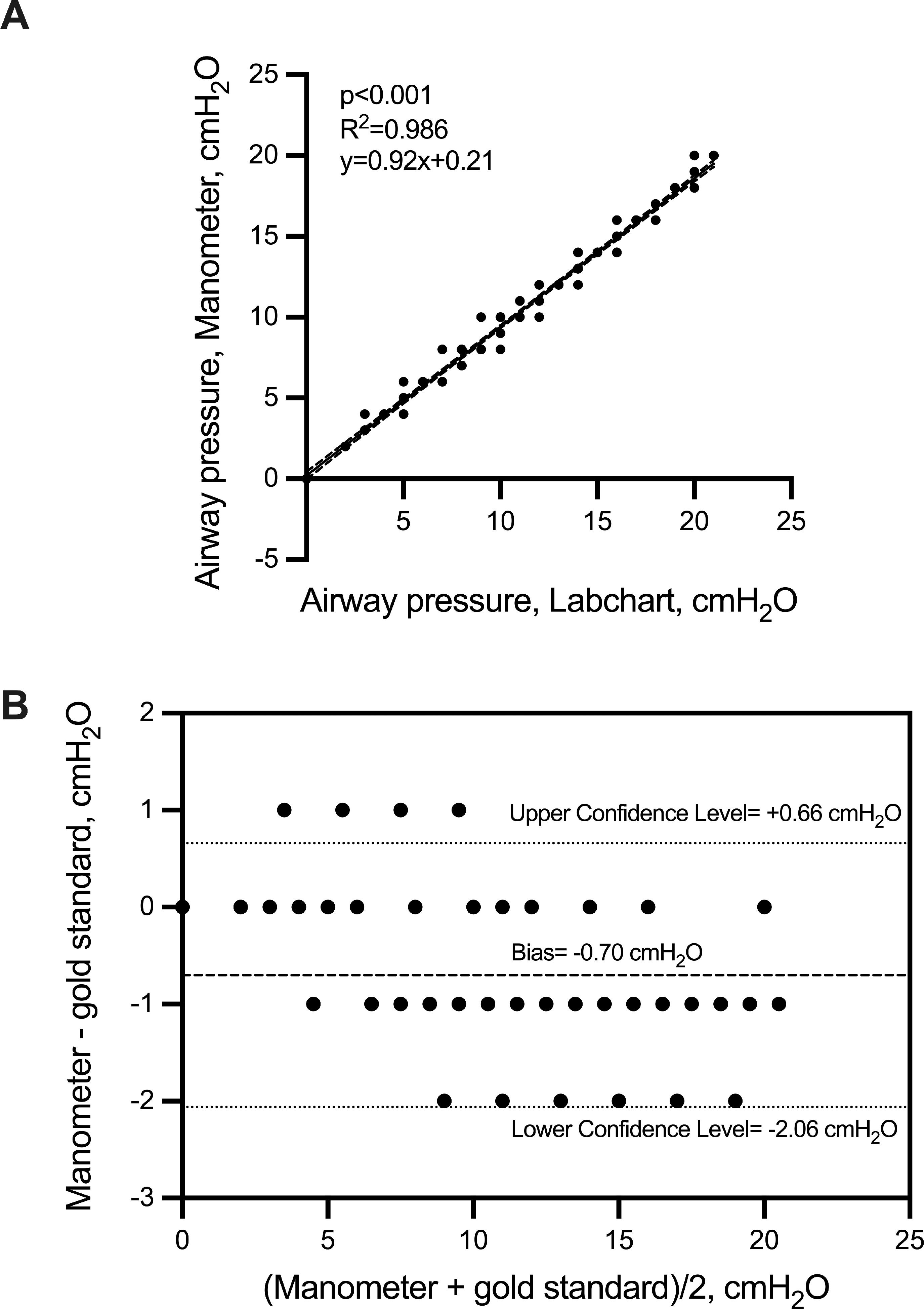
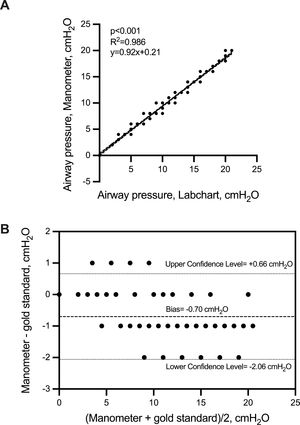
ResultsThe use of 8 different commercially available filters significantly increased the pressure within the hood of the CPAP helmet with or without the use of PEEP valves. On average, the increase of pressure above the set PEEP ranged from 3 cmH2O to 10 cmH2O across gas flow rates of 60 to 100 L/min. The measure of airway pressure was highly correlated between the laboratory pressure transducer and the Helmet manometer. Bias with 95% Confidence Interval of Bias between the devices was 0.7 (-2.06; 0.66) cmH2O.
ConclusionsThe use of HEPA and HMEF filters placed before the PEEP valve at the expiratory port of the CPAP helmet significantly increase the levels of airway pressure compared to the set level of PEEP. The manometer can detect accurately the airway pressure in the presence of HEPA and HMEF filters in the helmet CPAP and its use should considered.
Helmet continuous positive airway pressure (CPAP) was considered a useful and effective treatment in COVID-19 hypoxemic respiratory failure outside the Intensive Care Unit (ICU).1 The use of non-invasive ventilation (NIV) helped to avoid intubation by reducing complications associated with invasive mechanical ventilation.2-5 Ideally, COVID-19 patients should be admitted to hospital in a negative pressure room in order to prevent the contamination coming from the outside environment.6-8 In this context, Helmet CPAP would reduce the environmental spread of Sars-CoV2.9,10 Helmet CPAP is composed of a flexible plastic hood attached to a stiff plastic ring surrounding a soft plastic collar. The continuous gas flow of CPAP is guaranteed by a flow generator that blends together a gas mixture composed of ambient air (Air) and pure oxygen. In order to prevent CO2 rebreathing and to maintain a stable level of PEEP throughout the entire respiratory cycle, the gas flow should be at >50 L/min.11,12 PEEP is obtained by the use of expiratory valves that serve as gas flow resistors.13 Helmet CPAP decreases significantly the air leaks compared to the total face-mask14 and expired gas flow can be purified thanks to specific filters at the outlet of the helmet (i.e. High Efficiency Particulate Air filter – HEPA; and Heat & Moisture Exchanger Filter - HMEF). HEPA and HMEF filters have a hydrophobic membrane composed of glass fibers and confer a high antiviral and anti-bacterial efficiency (i.e. 99.999%).15 By using these filters, helmet CPAP is superior compared to other non-invasive respiratory devices in decreasing the virus dispersion.8,9,16 Unfortunately, the gas flow delivered through the helmet CPAP is rarely measured. The pressure within the hood may be considerably under estimated despite the level of pressure set on the PEEP valve.17 This phenomenon may be amplified in the presence of HEPA and HMEF filters placed before the PEEP valve.
We hypothesized that HEPA and HMEF filters - used before the PEEP valve for environmental protection against Sars-CoV2 dispersion, may act as a resistor and may greatly increase the airway pressure. The primary aim of the current study is to assess whether different HEPA and HMEF commercial filters may increase the airway pressure in the helmet CPAP above set levels of PEEP. This aim was tested using increasing levels of fresh gas flow. The secondary aim was to test the reliability of the reading system of airway pressure attached to the helmet CPAP (i.e. manometer) by comparing it with a calibrated pressure transducer.
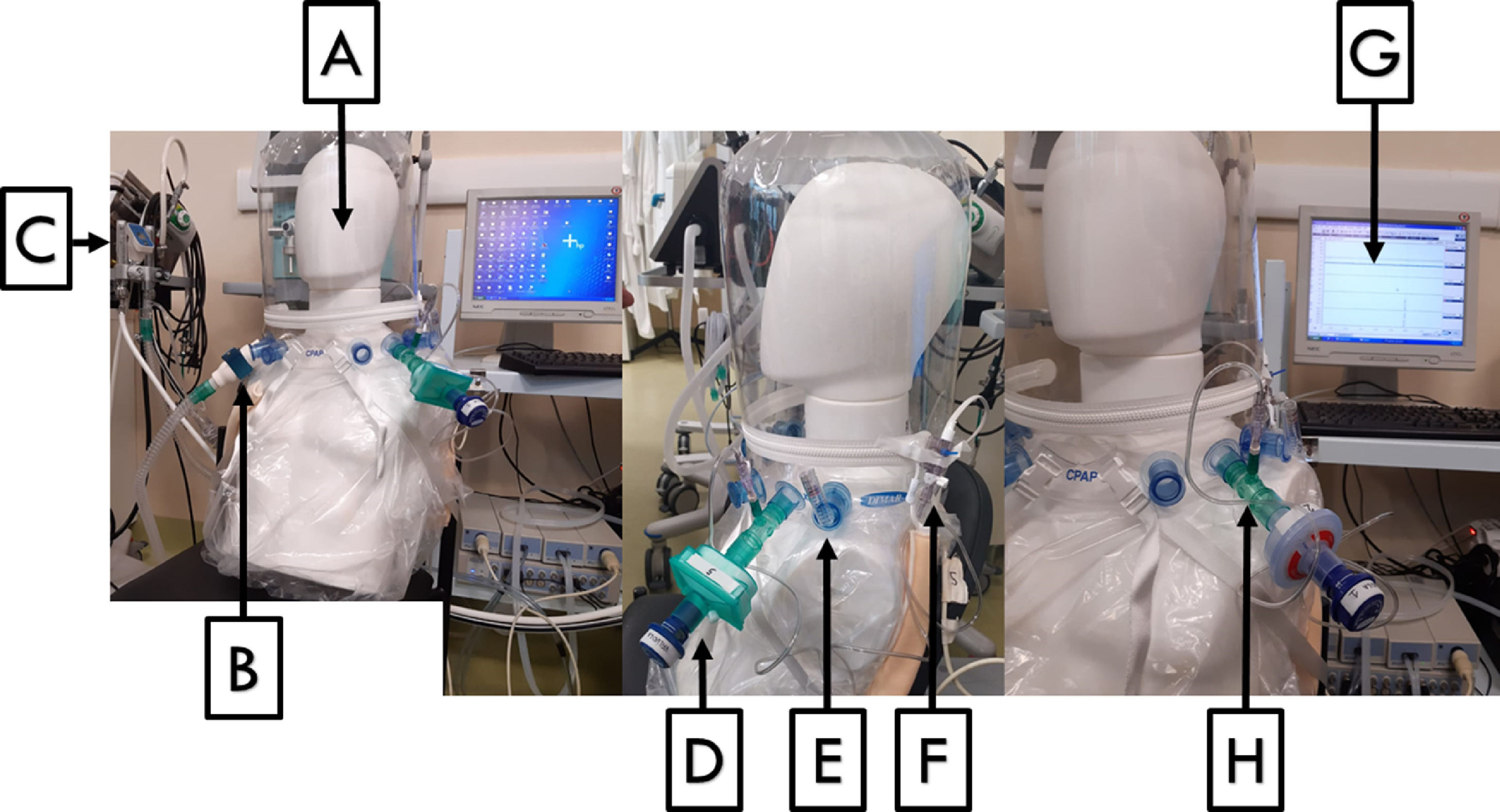
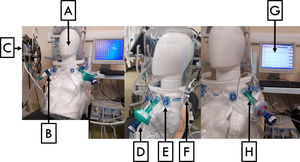
Materials and methodsThe hood of a commercially used helmet CPAP (DIMAR S.r.l. Via Galilei 6, 41036 Medolla Italy – mod. DimAir 500/9666) was placed on a mock manikin head and connected to a flow generator (EasyMIX by flow-meter Made in Italy – SN 00GMCZ), by a tubing connector (MALLINCKRODT DAR S.r.l., via G. Bove, 41037 Mirandola Modena - mod. 285/5063). The exit line of the hood was configured by using 2 different mechanical PEEP valves (DEAS valve - Deaflux Respiratory Production - NS 03986 [PEEP valve 1]; DIMAR Valve - DimAir mod. 700/6336 [PEEP valve 2]) and 8 different commercially available mechanical filters, 2 of them were HEPA and 6 of them were HMEF (Table 1). A calibrated pneumotachograph (ADINSTRUMENTS PowerLab 16/30 – Model: ML141 Serial 141-0990) was used to measure gas flow (Liter/sec). A pre-calibrated pressure transducer to atmospheric pressure was used to measure the pressure within the hood of the helmet CPAP (i.e. airway pressure) (EDWARDS LIFESCIENCE - Irvine, CA 92614 – Truwave PX260). The pressure transducer was placed at the exit line of the hood and connected to the acquisition system. At the same time, the levels of airway pressure were recorded by the manometer of the hood and reported in cmH2O (DIMAR S.r.l. – DimAir manometer mod. 700/6355) included in the helmet kit box. (Fig. 1). The pressure and flow tracings were recorded by a dedicated software and stored for off line analysis (“LABCHART” (ADINSTRUMENTS LabChart®7 v 7.2 Copyright ©1994-2010). We investigated the levels of airway pressure generated by different HEPA and HMEF filters in the absence of a PEEP valve (PEEP=0 cmH2O, zero PEEP, ZEEP) or in the presence of two levels of PEEP (i.e. 5 and 10 cmH2O) by using two commercially available mechanical PEEP valves, and 3 increasing levels of gas flow were tested (i.e. 60, 80 and 100 L/min). As first, we evaluated the airway pressure by using all studied HEPA and HMEF filters without the presence of a PEEP valve in order to assess whether the airway pressure could change by increasing the fresh gas flow. Subsequently, we explored the change in airway pressure levels by increasing fresh gas flow in the presence of 2 levels of PEEP (i.e. 5 and 10 cmH2O) and by using two different mechanical PEEP valves. For each step, we investigated the association between airway pressure levels measured by using the pressure transducers placed in the hood and the pressure manometer of the helmet CPAP.
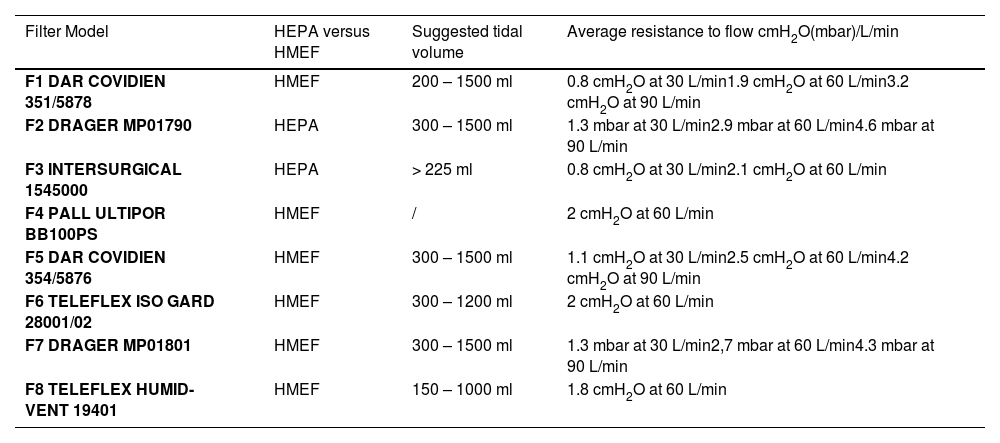
Technical specifics of HEPA and HMEF filters.
Data source: DAR COVIDIEN 351/5878 - https://www.medtronic.com/content/dam/covidien/library/ca/en/product/acute-care-ventilation/CA-PMR-0401-E-DAR-Filter-Catalog.pdf
DRAGER MP01790 - https://www.draeger.com/Products/Content/TwinStar-brochure-9066151-en-master_AFO.pdf
INTERSURGICAL 1545000 - https://www.intersurgical.com/products/airway-management/clearguard-range-medium-efficiency
PALL ULTIPOR BB100PS - https://shop.pall.com/us/en/products/zidBB100A
DAR COVIDIEN 354/5876 - https://www.medtronic.com/content/dam/covidien/library/ca/en/product/acute-care-ventilation/CA-PMR-0401-E-DAR-Filter-Catalog.pdf
TELEFLEX ISO GARD 28001/02 - https://www.teleflex.com/usa/en/product-areas/anesthesia/airway-management/passive-humidification-and-filtration/gibeck-iso-gard-filters/index.html
DRAGER MP01801 - https://www.draeger.com/Products/Content/TwinStar-brochure-9066151-en-master_AFO.pdf
TELEFLEX HUMID-VENT 19401 - https://www.teleflex.com/usa/en/product-areas/anesthesia/airway-management/passive-humidification-and-filtration/gibeck-hmefs/index.html
Helmet CPAP in vitro configuration. A) Helmet CPAP; B) Pneumotachograph place at the inlet of the helmet; C) Gas flow generator; D) Mechanical PEEP valve with HEPA/HMEF filter; E) Manometer; F) Pressure transducer; G) Acquisition system and pressure and flow tracings; H) airway pressure reading point.
Continuous variables were expressed as median with interquartile range (25th-75th percentile). Normality of distribution was assessed by using the Shapiro-Wilk test. Given the design of the bench study, differences in continuous variables across increasing levels of fresh gas flow (i.e. 60, 80 e 100 L/min) were tested by using the non-parametric test for repeated measurements Friedman's test. Post-hoc comparison across different flow rates was assessed by using the Benjamini, Krieger e Yekuteli test. The correlation between the levels of pressure measured by using the pressure transducer and the manometer of the helmet CPAP was evaluated by a linear regression using the Pearson's correlation coefficient. Analysis of agreement between the manometer placed on the helmet CPAP and the gold standard used to measure the pressure by using a pressure transducer was performed by using the Bland-Altman analysis. Bias with 95% confidence interval (CI) was reported. Statistical significance was set at a two-tailed p-value<0.05. Statistical analyses were performed using STATA/MP 17.0 for Mac (StataCorp, College Station, TX 77845, USA) and GraphPad Prism 9 for MacOs (Version 9.3.1, GraphPad, GraphPad Software, Inc.).
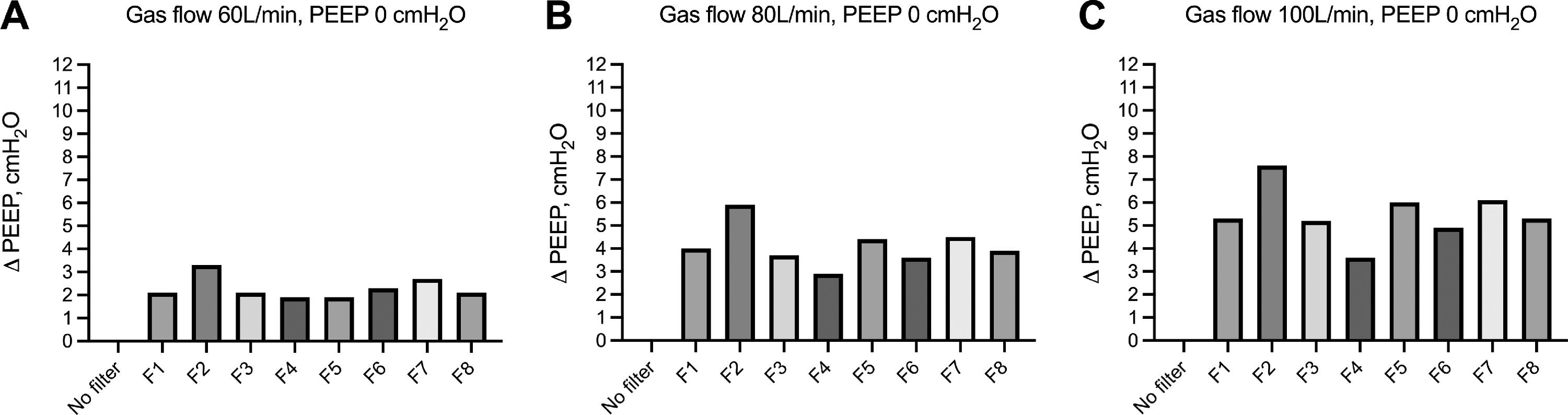
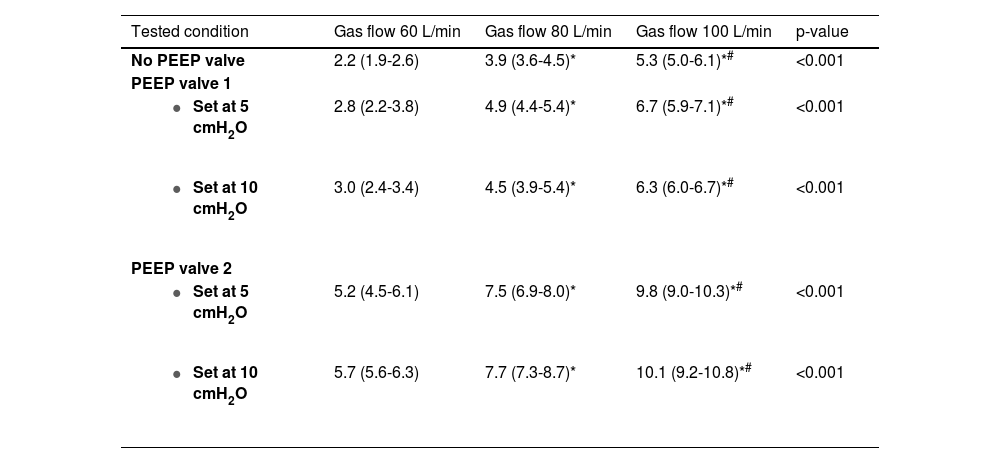
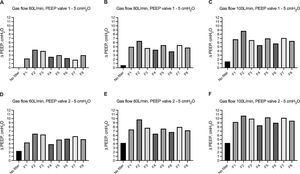
ResultsHEPA and HMEF filters gradually increase airway pressure at zero PEEP (ZEEP)We evaluated the change of airway pressure within the hood of the helmet CPAP with and without HEPA and HMEF filters in the absence of PEEP (i.e., ZEEP). As compared to atmospheric pressure, as expected the absence of HEPA and HMEF filters resulted in 0 ΔZEEP. In contrast, the use of HEPA and HMEF filters led to a gradual increase in ΔZEEP across increasing levels of gas flow, specifically ranging between 1.9-3.3 cmH2O, 2.9-5.9 cmH2O, to 3.6-7.6 cmH2O, at 60, 80 and 100 L/min of fresh gas flow, respectively (Fig. 2). We further evaluated the average effect on airway pressure of all HEPA/HMEF filters – as aggregate data in the absence of a PEEP valve - across increasing gas flow rates. Median increase ranged from 2.2 to 5.3 cmH2O (Table 2 and Supplemental Figure 1).
Change in airway pressure within the hood of the helmet CPAP (ΔZEEP) without and with different HEPA and HMEF filters across increasing gas flows and in the absence of a mechanical PEEP valve. Increasing flow rates are reported in from panel A – 60 L/min; to panel B – 80 L/min; to panel C, 100 L/min. Description of HEPA and HMEF (i.e. from F1 to F8) filters are reported in Table 1. Histobars summarize median and interquartile range.
Change in airway pressure (ΔPressure, cmH2O) over increasing gas flows and without using any PEEP valve and by using 2 different commercially available PEEP valves (PEEP valve 1 and 2).
ΔPressure are reported in cmH2O as median and interquartile range. p-value of the Friedman's test. * p < 0.05 versus 60 L/min. # p < 0.05 versus 80 L/min.
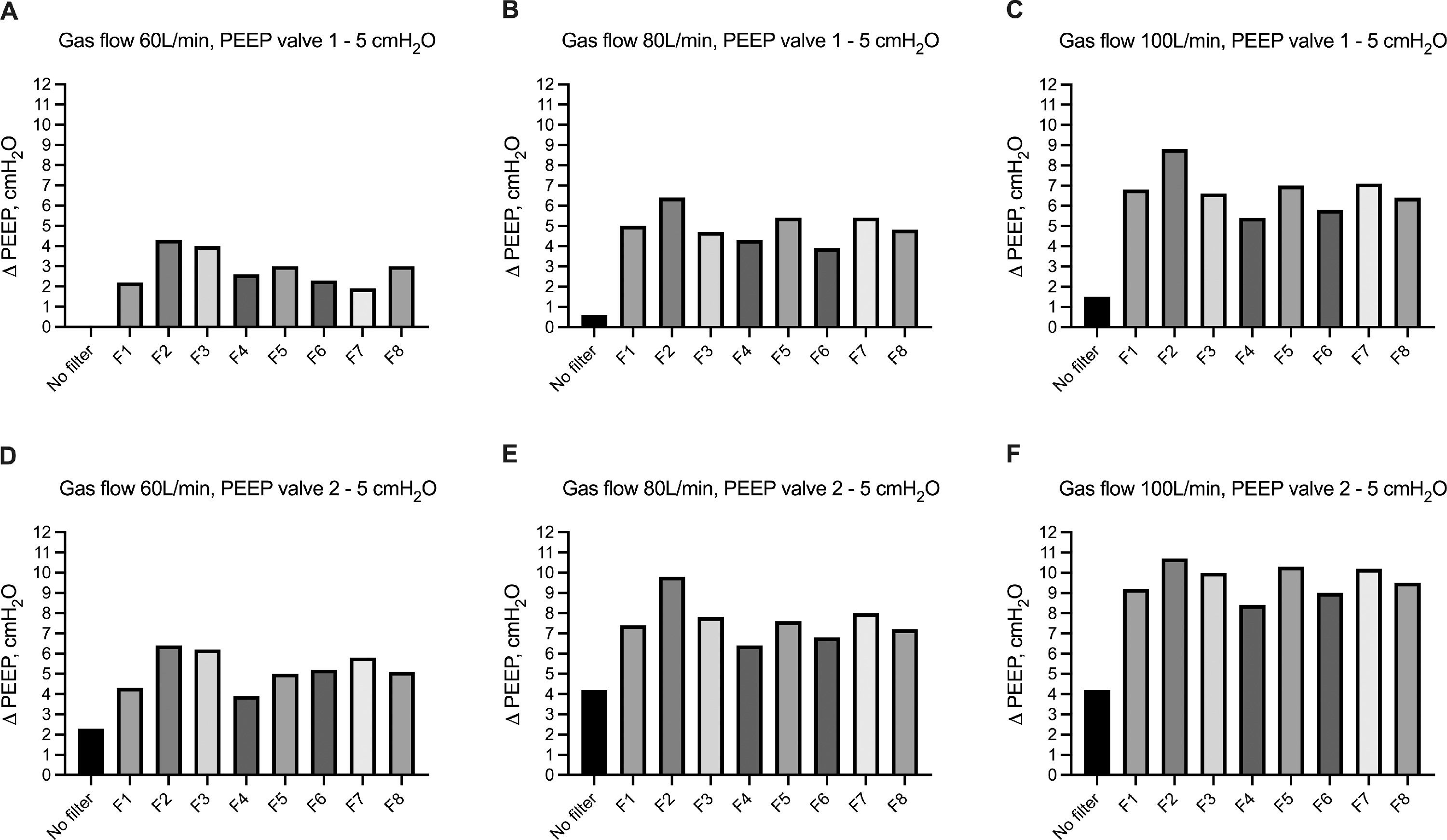
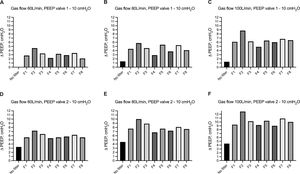
We evaluated the change of airway pressure within the hood of the helmet CPAP with and without HEPA and HMEF filters in the presence of PEEP=5 cmH2O with 2 different mechanical PEEP valves (i.e. valve 1 and valve 2). Using valve 1, as compared to set airway pressure at 5 cmH2O, the absence of HEPA and HMEF filters resulted in a ΔPEEP ranging from 0 to 1.5 cmH2O at increasing flow rates. The use of HEPA and HMEF filters led to a gradual increase in ΔPEEP across increasing levels of gas flow ranging between 1.9-4.3 cmH2O, 3.9-6.4 cmH2O, to 5.4-8.8 cmH2O, at 60, 80 and 100 L/min of fresh gas flow, respectively (Fig. 3a). We observed a similar effect using a different mechanical PEEP valve (i.e. valve 2). In the absence of HEPA and HMEF filters, ΔPEEP ranged from 2.3 to 4.2 cmH2O at increasing flow rates. The use of HEPA and HMEF filters led to a gradual increase in ΔPEEP across increasing levels of gas flow ranging between 3.9-6.4 cmH2O, 6.4-9.8 cmH2O, to 8.4-10.7 cmH2O, at 60, 80 and 100 L/min of fresh gas flow, respectively (Fig. 3b). We further evaluated the average effect on airway pressure of all HEPA/HMEF filters – as aggregate data in the presence of PEEP valve set at 5 cmH2O using both types of valves (i.e. valve 1 and vale 2) - across increasing gas flow rates. Average increase in ΔPEEP ranged from 2.8 to 6.7 cmH2O and from 5.2 to 9.8 cmH2O using PEEP valve 1 and PEEP valve 2, respectively (Table 2 and Supplemental Figure 2).
Change in airway pressure within the hood of the helmet CPAP (ΔPEEP) without and with different HEPA and HMEF filters in presence of mechanical PEEP set at 5 cmH2O. Increasing flow rates – from 60 L/min to 100 L/min - are reported in from panel A to panel C by using a) PEEP valve 1, and from Panel D to panel F by using PEEP valve 2. Description of HEPA and HMEF (i.e. from F1 to F8) filters are reported in Table 1. Histobars summarize median and interquartile range.
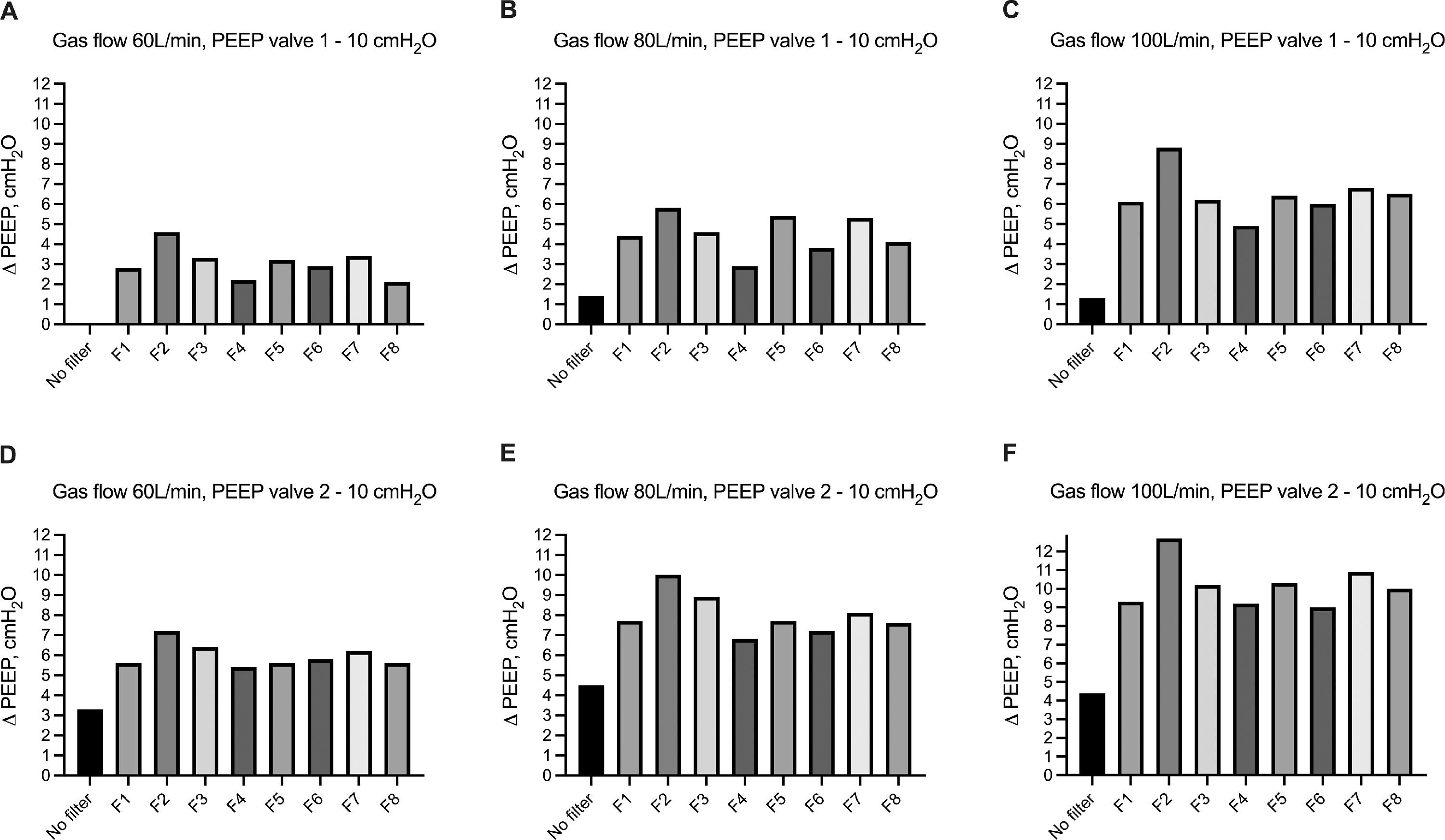
We evaluated the change of airway pressure within the hood of the helmet CPAP with and without HEPA and HMEF filters in the presence of PEEP=10 cmH2O with 2 different mechanical PEEP valves (i.e. valve 1 and valve 2). Using valve 1, as compared to set airway pressure at 10 cmH2O, the absence of HEPA and HMEF filters resulted in a ΔPEEP ranging from 0 to 1.3 cmH2O at increasing flow rates. The use of HEPA and HMEF filters led to a gradual increase in ΔPEEP across increasing levels of gas flow ranging between 2.1-4.6 cmH2O, 2.9-5.8 cmH2O, to 4.9-8.8 cmH2O, at 60, 80 and 100 L/min of fresh gas flow, respectively (Fig. 4a). We observed a similar effect using a different mechanical PEEP valve (i.e. valve 2). In the absence of HEPA and HMEF filters, ΔPEEP ranged from 3.3 to 4.4 cmH2O at increasing flow rates. The use of HEPA and HMEF filters led to a gradual increase in ΔPEEP across increasing levels of gas flow ranging between 5.4-7.2 cmH2O, 6.8-10.0 cmH2O, to 9.2-12.7 cmH2O, at 60, 80 and 100 L/min of fresh gas flow, respectively (Fig. 4b). We further evaluated the average effect on airway pressure of all HEPA/HMEF filters – as aggregate data in the presence of PEEP valve set at 10 cmH2O using both types of valve (i.e. valve 1 and vale 2) - across increasing gas flow rates. Average increase in ΔPEEP ranged from 3.0 to 6.3 cmH2O and from 5.7 to 10.1 cmH2O using PEEP valve 1 and PEEP valve 2, respectively (Table 2 and Supplemental Figure 3).
Change in airway pressure within the hood of the helmet CPAP (ΔPEEP) without and with different HEPA and HMEF filters in presence of mechanical PEEP set at 10 cmH2O. Increasing flow rates – from 60 L/min to 100 L/min - are reported in from panel A to panel C by using PEEP valve 1, and from Panel D to panel F by using PEEP valve 2. Description of HEPA and HMEF (i.e from F1 to F8) filters are reported in Table 1. Histobars summarize median and interquartile range.
We tested the association between the airway pressure with the pressure transducer on within the hood and the manometer placed on the helmet CPAP across all the steps performed at different gas flow rates (60, 80 and 100 L/min) and with different HEPA/HMEF filters and in the absence of PEEP (i.e. ZEEP) or at PEEP of 5 and 10 cmH2O. The correlation between the 2 measurements was very robust (r = 0.993, p < 0.001) (Fig. 5, panel A). Agreement between the 2 devices was good with a bias less than 1 cmH2O and a 95% CI within 3 cmH2O (Fig. 5, panel B).
Correlation (panel A) and agreement (panel B) between pressure levels measured by using a pre-calibrated pressure transducer and Helmet manometer. Panel A. Linear correlation (continuous line) with 95% CI (dotted line) between pressure levels measured by using a pre-calibrated pressure transducer (i.e. gold standard) and a manometer positioned on the helmet CPAP. Two-sided p-value, R2, and the equation of the fitted linear regression are reported; n=134. Panel B. Bland Altman plot with Bias and 95% Confidence Interval representing agreement between the 2 techniques performed to measure airway pressure within the helmet CPAP (i.e. Upper and Lower Confidence Level).
In this bench-top study, we investigated whether HEPA and HMEF filters placed at the expiratory port of the helmet CPAP may play a role in changing airway pressure within the hood in the presence of a set level of PEEP.
The primary findings of this study were that HEPA and HMEF filters – aimed at preventing microorganism dispersion – increase airway pressure in the helmet CPAP. The increment in airway pressure increases with the gas flow rate. This finding confirms that HEPA and HMEF filters act as resistors to fresh gas flow and significantly increase the airway pressure. This finding is concerning as it suggests that without a strict monitoring of the airway pressure in the helmet CPAP, the set level of PEEP may be unreliable. Furthermore, – as observed in this study – HEPA and HMEF filters may greatly underestimate the real pressure developed in the helmet CPAP. We reported that in the presence of high flow rates of fresh gas delivered through the helmet, we may easily double the set level of PEEP. This may lead to a dramatic increase in the risk of barotrauma which may further worsen the outcome of patients with respiratory failure.18 In a recent case series published in 2020, the authors reported that COVID-19 patients – more often male – may be inclined to develop spontaneous pneumomediastinum or pneumothorax.19,20 In other reports, the development of barotrauma has been reported in COVID-19 patients in all modalities of ventilation such as spontaneous breathing,21,22 NIV23 or in controlled mechanical ventilation.24,25 In this context, the potential increase of airway pressure determined by HEPA/HMEF filters may promote barotrauma.
Our study demonstrated that all studied HEPA/HMEF filters generated additive levels of pressure to the set levels of PEEP. This may make their use unpredictable and unsafe with the risk of inappropriate airway pressure delivery in the absence of an accurate pressure monitoring system. This was observed even at the lowest tested flow rate of 60 L/min. The increase of pressure determined by the HEPA and HMEF filters across increasing levels of flow, suggested that the increase of pressure within the helmet is determined by both HEPA/HMEF filters on one hand, and - on the other hand - by the type of PEEP valve used in the CPAP system.18
The second finding of the study is that the manometer used with the CPAP helmet is accurate and provides reliable measurements of the airway pressure within the CPAP helmet as compared to the gold standard (i.e. calibrated pressure transducer) in the presence of HEPA/HMEF filters. Furthermore, agreement between the two technique was good and clinically acceptable (i.e., Bias less than 1 cmH2O). This was reported with and without mechanical PEEP valve. This is a clinically relevant result that suggests that using the manometer on the CPAP helmet in daily clinical practice can reliably provide immediate information on the real airway pressure developed within the CPAP helmet at the end of expiration. Furthermore, this may suggest whether the modality of ventilation (i.e., gas flow, level of PEEP) should be changed and / or optimized.
Study limitationThis study has some limitations that should be acknowledged. First, this is a bench top study and the findings were not validated in the humans. Second, we evaluated 8 HEPA/HMEF filters commercially available, 2 different mechanical PEEP valve and one type of helmet CPAP on the market. We should then consider that our findings cannot be representative of all the types of filters, PEEP valves and helmets available on the market. This study it aims at raising awareness about the potential risk of barotrauma during the ventilation of patients with helmet CPAP that may have a role on their outcome. Furthermore, as this is an in vitro study - with the aim of providing precision and reproducibility of the results - it further aims at evaluating differences in the levels of airway pressure using a continuous flow. However, cyclic changes of flow were not part of this investigation.
ConclusionsIn this bench study, the use of HEPA and HMEF filters on the expiratory port of the helmet CPAP can increase the resistance to the continuous airflow with the consequent increase of the airway pressure within the hood. The use of a manometer applied to the helmet CPAP can provides accurate and reliable measurements of the airway pressure within the helmet CPAP as compared to a calibrated pressure transducer. Airway pressure generated within the helmet should be closely monitored in order to confirm that its levels matched with the targeted level of PEEP.
Authors’ contributionER, AL, RF, GB and GF: Conceptualization and Methodology, writing original draft. ER, GC, AG, LD, GPG and AL: data curation and validation. ER, GB and AL: formal analysis. All authors have read and approved the final manuscript.
None.
The present study was performed at the General Intensive Care Unit, Emergency Department and Intensive Care, San Gerardo Hospital – ASST Monza, Via Pergolesi 33 – Monza (MB), Milan-Bicocca University – Italy.