Obesity, defined by a body mass index (BMI) ≥30kg/m2, is associated with an increased risk of several diseases and is a major risk factor for the development and progression of Obstructive Sleep Apnea (OSA).1 The interaction between OSA and obesity is complex. On one hand, there are forces that promote airway collapse as the intraluminal negative pressure and the extraluminal pressure exerted by tissues and bone structures surrounding the airway2 and on the other, these forces are opposed by the action of pharynx muscles and by the longitudinal traction exerted in the airway by the rise of lung volume. In obesity, the deposition of periluminal fat and the reduction of lung volume contribute to an altered compliance of the upper airway thus promoting its collapse.2 During sleep there is a physiological decrease in the tone of the pharynx muscles that induce a slight narrowing of the upper airway3 which, in the case of obese individuals, contributes to a further reduction of the pharynx lumen leading to OSA symptoms. One of the most important symptoms is the excessive daytime sleepiness4 which is believed to be caused by sleep fragmentation. This characteristic of OSA patients can contribute to a reduced level of physical activity and energetic metabolism predisposing to obesity. Moreover, studies suggest that genetic polymorphisms of the leptin receptor may influence both sleep apnea and obesity,1 contributing to metabolic dysregulation in these patients.
The treatment of obese patients with OSA involves behavioral changes, positive airway pressure and bariatric procedures: intragastric balloon and bariatric surgery. This is the more effective current treatment for morbidly obese5 and produces a sustained weight loss, being associated with a better possibility of cure of OSA.
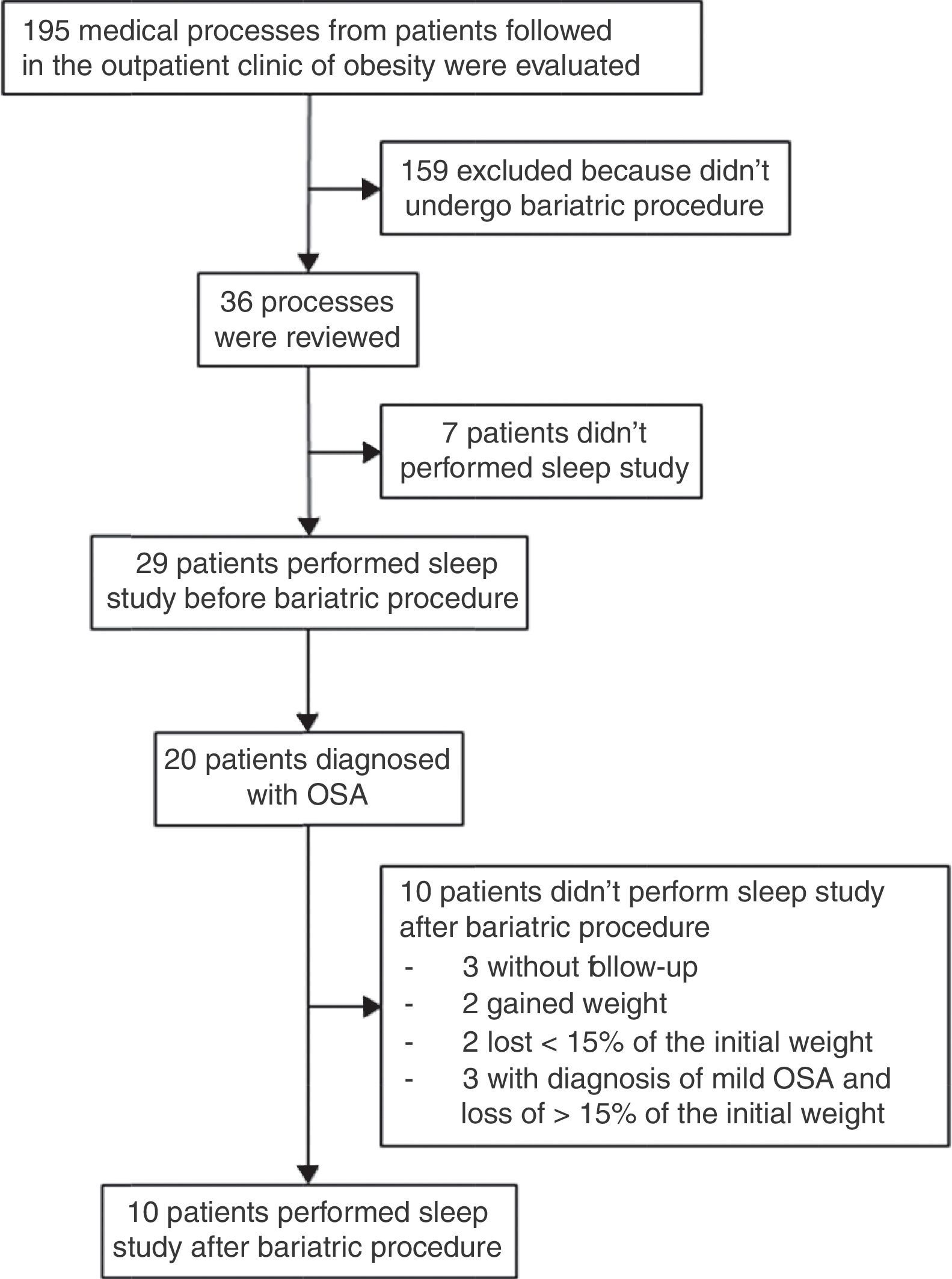
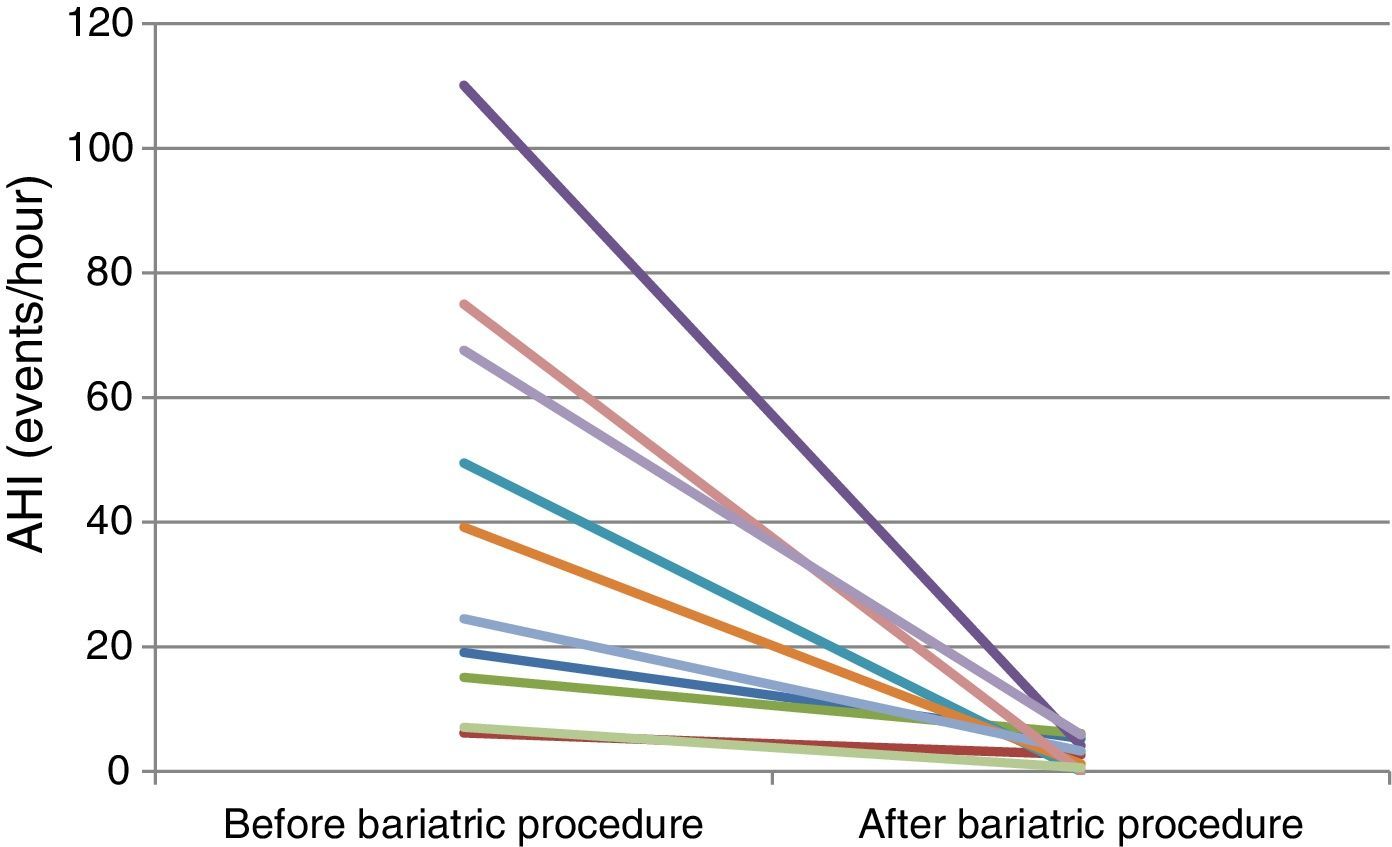
To assess the impact of weight loss on OSA in obese patients who underwent bariatric procedure, a retrospective study was conducted in Santa Maria Hospital (HSM), North Lisbon Hospital Center (CHLN). Data was collected on patients with a BMI ≥35kg/m2 who underwent bariatric procedure (Fig. 1). Thirty-six patients were included, 30 (83%) were female; the mean age was 43.3±9 years and the mean BMI was 46.9±6.2kg/m2. Males had a higher BMI than females. Of the twenty-nine patients tested with polysomnography before surgery due to symptoms associated with OSA, 20 were identified with OSA. Of these, 10 repeated the polysomnography 12±7 months after bariatric surgery. Seven patients were female and the mean age was 46.3±9.5 years. The mean BMI fell from 48.3±7.5kg/m2 to 32.9±6.3kg/m2 with a mean loss of excess weight of 56.2±21.8%. Six patients lost more than 50% of excess weight. There was a resolution of OSA in seven patients and a significant improvement was noted in the other three. A significant reduction of apnea hypopnea index (AHI) was noted from a median value of 31.9/h to 3/h. There was a significant improvement in minimal peripheric oxygen saturation with a rise in the mean value from 73±3% to 86±4%. There was an improvement in the median value of total time of oxygen saturation below 90% (T90) from 32.5 to 1.2min. A significant reduction was noted in the median value of Oxygen Desaturation Index (ODI) from 45.5events/hour to 4.2events/hour.
Regarding the other 10 patients who did not repeat the sleep study, three abandoned the medical follow-up and two gained weight therefore it was assumed that there had been no improvement in the disease. Two patients failed to lose 15% of body weight after the bariatric procedure and considering they had moderate OSA and associated comorbidities it was assumed they would not benefit from repeating the sleep study. Three patients lost more than 15% body weight after bariatric procedure and presented mild OSA in the pre-operative polysomnography with an AHI in the limit of normality (AHI 7.2/h; 5.6/h e 9.7/h), so there was no clinical need to repeat the sleep study.
Weight loss associated with bariatric procedure is beneficial for obese patients with OSA as shown by the significant reduction of AHI and other indexes related to OSA one year after the bariatric procedure. Besides behavioral treatment, which should be offered to every patient, long-term treatment with positive airway pressure is the treatment of choice for OSA.6 However, for morbid obesity, bariatric procedure should be considered as it produces effective results in weight loss which has a beneficial impact on OSA.
Conflicts of interestThe authors have no conflicts of interest to declare.