Obstructive sleep apnea (OSA), if left untreated, is associated with high cardio-vascular (CV) morbidity and mortality. Based on large-scale epidemiological studies, it is known that excessive sleepiness is a cardinal symptom but the majority of individuals with high Apnea Hypopnea Index (IAH) do not complain of it.1,2
Arterial stiffness, evaluated by pulse wave velocity (PWV), has a predictive value for CV events, beyond classical risk factors, and can be considered as an intermediate endpoint for CV events. Carotid-femoral pulse wave velocity (cf-PWV) remains the most commonly used non-invasive method and is considered as the gold standard.3
Increased PWV is associated with various conditions, of which age and blood pressure (BP) are the most important. In OSA cf-PWV value is augmented, with improvement after treatment with CPAP.4,5
In order to explore the association of sleepiness with CV risk in patients with OSA, we conducted a prospective study of consecutive males, younger than 65 years old, referred for snoring or OSA related symptoms. They were included if they had moderate to severe OSA (AHI>15) diagnosed by cardiorespiratory polygraphic study, level 3, in our institution's sleep laboratory, and excluded if they had other sleep disturbances, diabetes or CV disease beyond hypertension. Epworth Sleepiness Scale (ESS) score>10 defined excessive sleepiness. Patients with high BP in 24h monitoring (ABPM) or already taking antihypertensive drugs were considered hypertensive. Arterial stiffness was assessed by cf-PWV, and 10m/s was used as threshold value. CV risk was calculated by SCORE – European Low Risk Chart.
Univariable logistic regression and stratified Mantel–Haenszel analyses were performed to quantify associations between variables.
From approximately 700 patients referred to the Clinic during the study, 34 patients were recruited, with median age 53.0 years; 24 (70.6%) were hypertensive (15 with medication), 18 (52.9%) had metabolic syndrome and 30 (91%) had dyslipidaemia. The cf-PWV was high in 27 (79.4%) and the median SCORE CV risk was 2 (0–5), 26 out of 33 patients had moderate CV risk.
All patients with normal cf-PWV had moderate OSA, and cf-PWV was significantly higher when OSA was severe rather than moderate OSA (p=0.047). In fact, weak evidence was found that the odds for high cf-PWV increase with either increasing AHI (OR 1.08; 95%CI 0.99–1.18; p=0.078) or ODI (OR 1.14; 95%CI 0.98–1.32; p=0.086). No association was found between cf-PWV and ABPM measurements.
Patients with high cf-PWV also had similar prevalence rates of arterial hypertension (57.1% [95% CI 25.05–84.18] vs. 74.1% [95% CI 55.32–86.83]; p=0.394) but higher SCORE CV risk (median (maximum) 1 (2) vs. 3 (5); p=0.029).
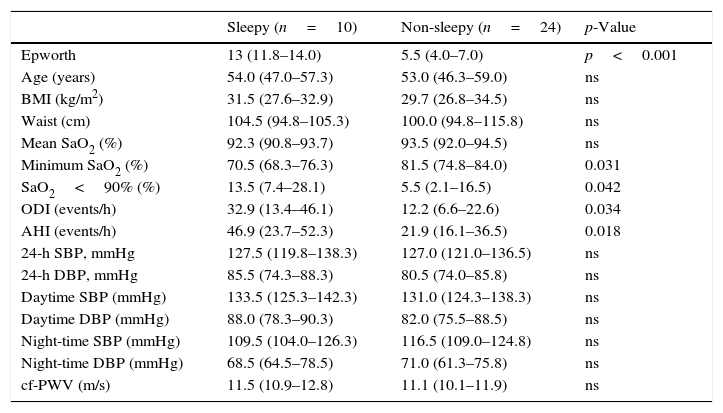
Excessive sleepiness was diagnosed in 10 (29.4%) patients which had significantly higher AHI, ODI and higher SaO2<90% but lower minimum SaO2 than non-sleepy patients (Table 1).
Clinical characteristics of the participants, classified by sleepiness group. Values are median and interquartile range (IQR).
| Sleepy (n=10) | Non-sleepy (n=24) | p-Value | |
|---|---|---|---|
| Epworth | 13 (11.8–14.0) | 5.5 (4.0–7.0) | p<0.001 |
| Age (years) | 54.0 (47.0–57.3) | 53.0 (46.3–59.0) | ns |
| BMI (kg/m2) | 31.5 (27.6–32.9) | 29.7 (26.8–34.5) | ns |
| Waist (cm) | 104.5 (94.8–105.3) | 100.0 (94.8–115.8) | ns |
| Mean SaO2 (%) | 92.3 (90.8–93.7) | 93.5 (92.0–94.5) | ns |
| Minimum SaO2 (%) | 70.5 (68.3–76.3) | 81.5 (74.8–84.0) | 0.031 |
| SaO2<90% (%) | 13.5 (7.4–28.1) | 5.5 (2.1–16.5) | 0.042 |
| ODI (events/h) | 32.9 (13.4–46.1) | 12.2 (6.6–22.6) | 0.034 |
| AHI (events/h) | 46.9 (23.7–52.3) | 21.9 (16.1–36.5) | 0.018 |
| 24-h SBP, mmHg | 127.5 (119.8–138.3) | 127.0 (121.0–136.5) | ns |
| 24-h DBP, mmHg | 85.5 (74.3–88.3) | 80.5 (74.0–85.8) | ns |
| Daytime SBP (mmHg) | 133.5 (125.3–142.3) | 131.0 (124.3–138.3) | ns |
| Daytime DBP (mmHg) | 88.0 (78.3–90.3) | 82.0 (75.5–88.5) | ns |
| Night-time SBP (mmHg) | 109.5 (104.0–126.3) | 116.5 (109.0–124.8) | ns |
| Night-time DBP (mmHg) | 68.5 (64.5–78.5) | 71.0 (61.3–75.8) | ns |
| cf-PWV (m/s) | 11.5 (10.9–12.8) | 11.1 (10.1–11.9) | ns |
Epworth – Epworth Sleepiness Scale; BMI – body mass index; SaO2 – arterial oxygen saturation; SaO2<90% – time under 90%; ODI – oxygen desaturation index; AHI – Apnoea-Hypopnoea Index; SBP – systolic blood pressure; DBP – diastolic blood pressure; cf-PWV – carotid-femoral pulse wave velocity.
Sleepy and non-sleepy patients did not differ in prevalence rates of hypertension (70.0% vs. 70.8%) or average BP values. However, all patients with normal average ABPM values under medication were non-sleepy. Both cf-PWV and SCORE CV risk were similar regarding sleepiness (median (maximum) 2 (4) vs. 2 (5); p=0.764). A weak evidence was found of a better control of BP with medication in non-sleepy patients, based on the ABPM values (Mantel–Haenszel, p=0.091).
Other authors reported similar relationships between sleepiness and cf-PWV in OSA. Drager et al.6 made an observational study of patients with metabolic syndrome, and Kohler et al.7 used a different arterial stiffness index.
In this sample of male patients without significant comorbidities, who are suspected by their primary care physician of having OSA and needing treatment, a high prevalence of arterial hypertension was found, common in OSA; It should be noted that in 25% of the sample it was previously undiagnosed and in 80% of the patients under drug therapy, it was uncontrolled. High BP was present regardless of sleepiness, but in non-sleepy patients it may be easier to control with medication.
This analysis had, as limitations, the small number of patients and the exclusion of patients with mild OSA, older patients or those patients with serious comorbidities.
In conclusion, sleepy patients have more severe OSA, they tend to be more hypertensive and have uncontrolled BP, but arterial stiffness and CV risk are similar in regard of sleepiness.
Conflicts of interestThe authors have no conflicts of interest to declare.