Serine/threonine kinase 11 gene (STK11) codes a kinase involved in the regulation of cell growth, polarity and motility, through phosphorylation of adenosine monophosphate-activated protein kinase (AMPK). Somatic mutations have been reported in up to 30% of Caucasian non-squamous non-small cell lung cancer (NSCLC) patients. STK11 mutations may assume oncogenic functions, associated to reduced survival in lung adenocarcinoma.1 We present a case of a STK11 mutated lung adenocarcinoma presenting a good outcome with immunotherapy.
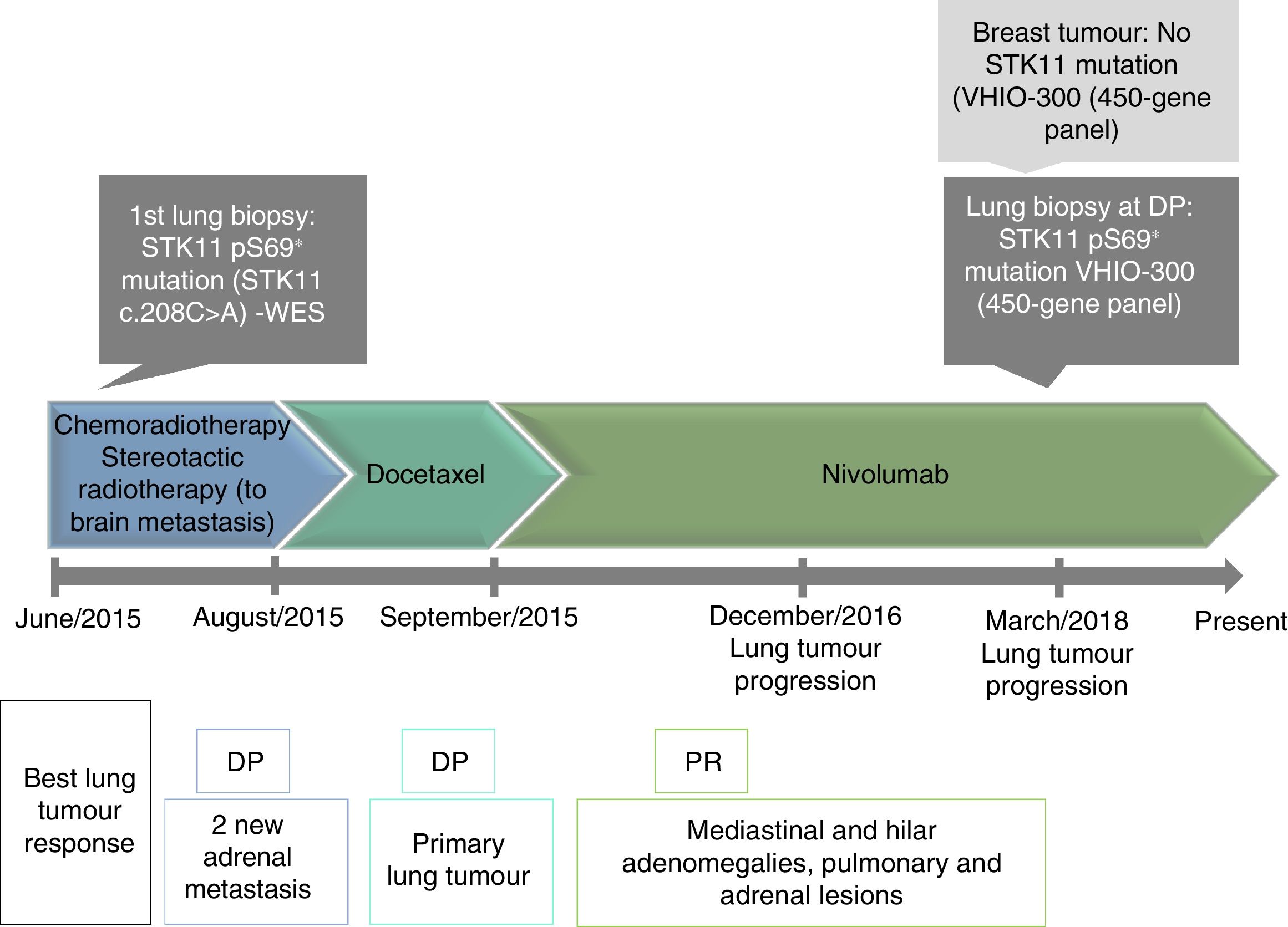
A 51-year-old female patient, light smoker, diagnosed in May/2015 with two synchronic tumours: lung adenocarcinoma cT2aN2M1c (one cerebellar asymptomatic lesion; EGFR wild-type, ALK/ROS1-, KRAS-, HER2-, PD-L1<1% by 22C3 assay); and breast invasive ductal carcinoma grade 3, cT2N0M0, hormonal receptors positive (ER 100%, PR 45%), HER2- and Ki-6740%. Whole exome sequencing of lung tumour showed a somatic S69* variant in STK11 gene (STK11 c.208C>A) at 27% allelic frequency, without additional targetable mutations, and a tumour mutational burden (TMB) of 4.9 mutations/megabase (<10 mutations/megabase).
She started chemoradiotherapy for lung cancer and stereotactic radiosurgery of cerebellar metastasis, as an oligometastatic NSCLC. After 2 months, disease progression (DP) was observed with new adrenal lesions.
Second line docetaxel was started, presenting DP of NSCLC after one month, but with breast cancer reduction.
In September/2015, the patient started a third line with nivolumab. Partial response was observed at two months and patient continued with the immunotherapy. After fifteen months lung and breast tumours increased, and local therapy was performed (stereotactic radiotherapy for lung, followed by breast lumpectomy, pT1cN0M0). Post-lumpectomy RT was considered to have no further benefit. She started adjuvant therapy with letrozole.
In March/2018, after thirty months, lung tumour had a second DP under immunotherapy, and underwent a new biopsy. At this point, this lung biopsy along the primary breast tumour were analysed through the VHIO-300 panel (450 genes) revealing presence of the STK11 mutation in lung at DP (52.4% mutant fraction) and complete absence of the variant in breast.
Despite DP, she remained asymptomatic, with good tolerance to nivolumab and letrozole. Immunotherapy proceeded until present (thirty-nine months), given the clinical benefit (Fig. 1).
In synchronous tumours, the most advanced assumes a prognostic importance. Although lung and breast tumours are common in females, their synchronous diagnosis is infrequent.2 The patient's tumours didn’t present a common mutational background.
Molecular classification of NSCLC has a direct impact on prognosis and treatment choices. STK11 is thought to have a role on pulmonary tumorigenesis, often associated with KRAS.3,4 The reported STK11 pS69* mutation results in a premature stop codon within its kinase domain, associated to more aggressive tumours, shorter progression-free survival and overall survival.1,3 Additionally, this mutation has been associated with significantly shorter time on PD-1/PD-L1 blockade therapy in NSCLC (or even resistance),3 possibly by reducing density of tumour infiltrating cytotoxic CD8+T lymphocytes.5 Despite the STK11 mutation, our patient presented a long survival and a clinical benefit from immunotherapy, as well as from thoracic radiotherapy and its possible abscopal effect.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors
Conflicts of interestThe authors have no conflicts of interest to declare.