Tunnelled indwelling pleural catheters (TIPC) are a modality of treatment for malignant pleural effusions. Though relatively easy, safe and efficacious, they are associated with a small risk of complications. We describe newer complications of the TIPC including the retention of the polyester plug and the blockage of the catheter with thick organised material consisting of malignant cells taking the shape of the catheter.
Tunnelled indwelling pleural catheters (TIPC) have gained a significant role in the ambulatory management of patients with malignant pleural effusions. The modern day TIPC consists of a multi-fenestrated chest drain of flexible silicone, with a small polyester cuff enveloping the medial portion of the tube. The latter part is tunnelled through subcutaneous tissue before the distal portion enters the pleural space, with the cuff acting as a focal point for fibrous growth to allow the drain to remain in place. At the proximal (external) end is a one-way access valve designed to be attached to proprietary vacuum drainage bottles.1 TIPC use is safe and efficacious but certain complications have been described.2 We describe two new and previously unreported complications of the TIPC.
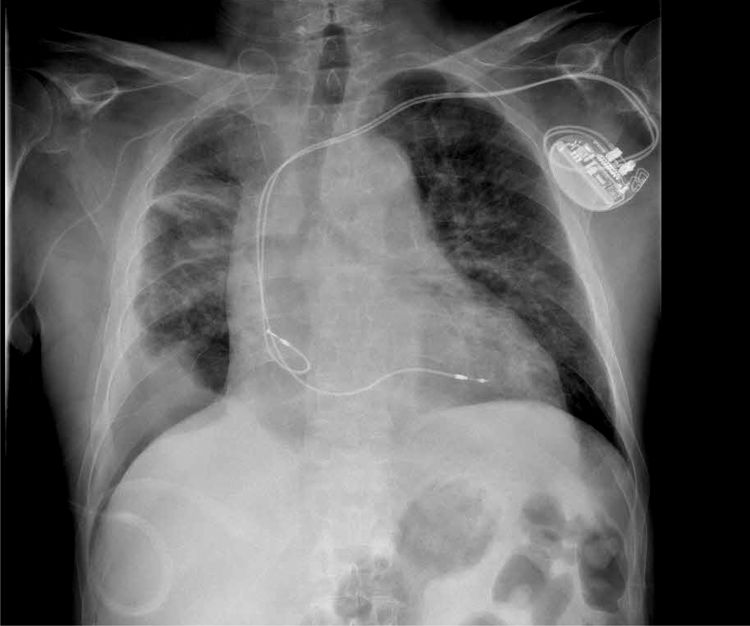
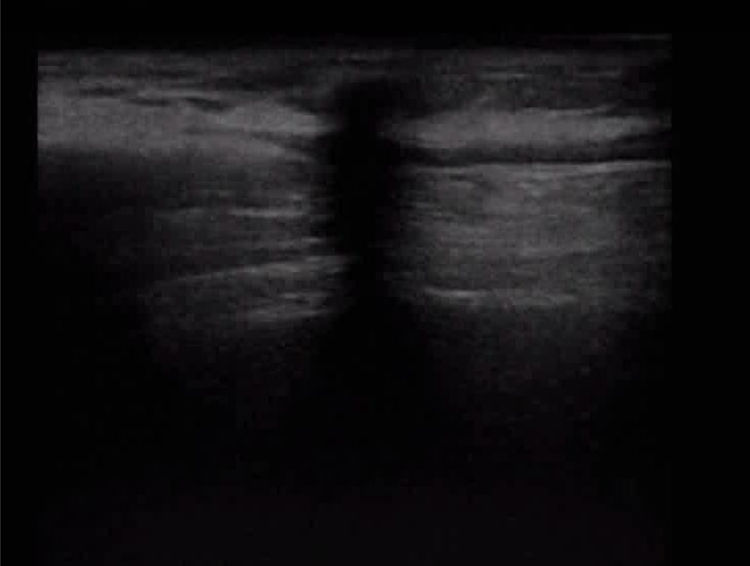
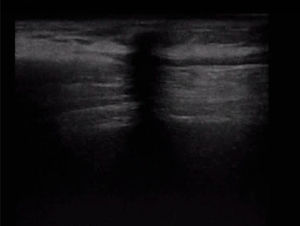
Case summaryCase 1. A 75 year old man was a known case of carotid vasculopathy on clopidogrel therapy, COPD with cor-pulmonale on oxygen therapy and hypertension. In 2017 he was evaluated and proved to have adenocarcinoma of lung (cT4 N3 M0-Stage IIIB), given symptoms of cough, dyspnoea and the chest radiograph and computed tomography (CT) of thorax suggestive of right lower hilar mass encasing the right main bronchus on bronchoscopy guided endobronchial biopsy. The patient was referred for oncology assessment and treated with chemotherapy, radiotherapy and later immunotherapy. In 2019, the patient presented with progression of the lung malignancy and a right recurrent pleural effusion which was managed with insertion of the TIPC. After two months of drainage the patient was referred back by the nurse due to nil drainage. In view of spontaneous pleurodesis and chest X-ray (CXR) showing right pleural thickening (Fig. 1), the catheter was removed. Post removal it was observed that polyester plug on the TIPC was missing (Fig. 2). An ultrasound of the local area showed a hypoechogenic spot in the medial tract of the previous tunnelling extending from the subcutaneous tissue down due to the acoustic shadow from the retained plug in the subcutaneous space (Fig. 3). As the patient was on antiplatelet therapy and material being inert; skin and subcutaneous tract dissection was not done. The patient and relatives were informed about the situation and he was sent home with the retained polyester plug.
Case 2. A 77 year old lady, a known case of breast cancer was managed with surgery, chemotherapy and radiotherapy in 1989, then with chemotherapy for chest wall metastasis in 2013. Subsequently she had lung nodules and a small right pleural effusion which was managed with further chemotherapy. In January 2019, she presented with dyspnoea and large metastatic left pleural effusion which was treated with TIPC. In view of non-functionality and CXR suggestive of residual small pleural effusion the IPC was removed after two months (Fig. 4). After removal and dissection of the old IPC, it was observed to be filled with a long, thick, haemorrhagic organised material, completely intact, taking the shape of the IPC and appearing like the plant “corallo rosso” (Fig. 5). The material on histopathological examination was positive for metastatic adenocarcinoma cells.
DiscussionTreatment of malignant pleural effusion is intended to be palliative, to relieve symptoms and improve quality of life. The two main approaches involve drainage followed by pleurodesis versus continuous drainage with TIPC. The former is preferred for patients with a longer life expectancy. But the latter is associated with fewer complications and shorter hospital stay.3 A TIPC is indicated in cases of malignant pleural effusion with symptoms, recurrent pleural effusions, where the patients have short to intermediate life expectancy or trapped lung or previous unsuccessful pleurodesis.4,5
TIPC has been reviewed as being safe and efficacious for management of malignant pleural effusions.6,7 Lui et al review in detail the complications of TIPC such as pleural infections, catheter tract metastasis, symptomatic loculations, nutrition and cell loss, fractures of catheter on removal, catheter blockage, chest pain and the costs of TIPC management. Catheter related pleural effusions were further sub divided into cellulitis, empyema and tunnel infections.9 Fysh et al reported complications in 9.8% cases of TIPC removal leading to fracture or iatrogenic severing and four patients having catheter fragments retained within the pleural space without any complications.10 Grosu et al describe the various reasons for fractures of TIPC such as, greater than 1cm placement of the catheter cuff within the tunnel, longer than 5cm subcutaneous tract, catheter tract metastasis, mesothelioma and changes in the manufacturing process of the catheters.2
Management of TIPC complications has been reviewed in literature. TIPC related pleural infections can be avoided by continual assessment of patient related, TIPC related and clinician related risk factors, including need for drainage and prompt removal when further drainage was not indicated. Patients with catheter tract metastasis have been treated with analgesia and external beam radiotherapy. Symptomatic loculations have been addressed with pleural aspiration or second catheter placement. General dietary care can cover the nutritional losses due to TIPC drainage. Catheter fractures can be avoided by careful removal, using less traction force. Retention of fractured fragments was not associated with any complications. Saline flush and manipulation along the catheter have been documented in literature to prevent catheter blockage. Chest pain required appropriate analgesia and withdrawal of negative suction if used.8
Polyester plug retention in the subcutaneous tissue was a novel complication associated with the TIPC and has never been reported before. The TIPC of our patient was removed intact without any signs of fractures or retained fragments which have been more commonly described. The polyester plug must have mostly organised due to dense fibrosis in the adjacent area and hence was retained on removal. While catheter blockage has been described in literature, our patient had the same thing due to a thick organised material consisting of blood and malignant cells which took a very fascinating shape like that of the plant “corallo rosso”.
Conflicts of interestThe authors have no conflicts of interest to declare.