Spirometry is a key component of the asthma management guidelines’ workup for diagnosis, assessment and monitoring of severity and control.1 However, evidence from practice pattern studies and surveys suggests there is limited use of spirometry in patients of all ages with asthma,2 for reasons that remain unclear.3,4 In Portugal, the National Program for Respiratory Diseases warns that this is also the case for chronic obstructive pulmonary disease.5
Our main objective was to evaluate and compare current knowledge and practice of spirometry prescription and interpretation among the four groups of physicians caring for children/adolescents with asthma in Portugal: Paediatricians (Ped), Pulmonologists (Pn), Allergologists (AI) and General Practitioners (GP). Secondary objectives were to identify determinants of spirometry prescription and limitations of use, and to assess the need for a training program.
MethodsStudy designThe EspiroPed survey was a cross-sectional electronic survey targeting Ped, Pn, AI and GP who follow asthmatic children/adolescents and work in Portugal. These were current members of their respective scientific societies i.e.: Sociedades Portuguesas de Pediatria, de Pneumologia e de Alergologia e Imunologia Clínica and Associação Portuguesa de Medicina Geral e Familiar. Each scientific society reviewed and approved the research protocol.
QuestionnaireA questionnaire on various topics of spirometry use in asthmatic children/adolescents was developed in Portuguese through informal consensus and with different response formats (multiple choice, 5-point Likert items and categories of frequency of use) (available as a supplementary appendix). We collected anonymized data on physicians’ training and workplace; knowledge of national asthma guidelines and ATS/ERS spirometry recommendations; accessibility to and practices of spirometry prescription. The survey was developed using the SurveyMonkey platform (www.surveymonkey.com) and was pilot tested for acceptability and feasibility.
ImplementationThe survey ran for six weeks in 2015 (July-August for Ped/Pn, and October-November for AI/GP) An invitation with an open link was sent to each society’s mailing list. Four reminder e-mailswere used to optimize the response rate. Consent was implied by survey completion. The Ethics Committee of Centro Académico de Medicina de Lisboa approved this study.
Statistical analysisDescriptive analysis, stratified by physician specialty, was performed on fully completed surveys. We compared results between physician specialties using univariable analysis (Chi-square test), considering a significance level of 5%. Statistical Package for the Social Sciences 21.0 (SPSS®, Chicago, USA) was used to perform all tests.
ResultsComplete responses were available from 423 physicians: 89 Ped, 40 Pn, 30 AI and 264GP (approximately 5–7% of eligible members from each Society). Most were specialists [241(57%)], worked in Lisbon [98(23%)] or Porto [92(22%)] and in public hospitals/clinics [269(64%)]. Non-asthma chronic respiratory diseases were managed by 58% Ped, 65% Pn, 70% AI, 62% GP (p=0.6). Overall, only 17(4%) reported having had training in Paediatric Respiratory Medicine.
No differences were found between groups concerning knowledge of national asthma guidelines. The majority of Pn/AI (90%/93%) knew the ATS/ERS guidelines on spirometry compared to only 30%Ped and 19%GP (p<0.001) and, accordingly, 53%Pn and 37%AI also mentioned having “very good knowledge” of how to perform a spirometry, as opposed to 7%Ped and 3%GP (p<0.001). All groups agreed that besides age, comprehension and collaboration were the most important factors to be taken into consideration when performing spirometry in children. Most physicians considered 6 years of age or below to order spirometry, and the majority preferred public/state laboratories (72% Ped, 55% Pn, 63% AI and 62% GP). Regarding the interpretation of spirometry, 65%Pn and 70%AI reported having “very good knowledge” compared to 10%Ped and 5%GP (p<0.001). No differences among groups were found on which parameters (FEV1, FVC, FEV1/FVC, FEF25–75%, morphology of the flow-volume loop) were used when interpreting a spirometry.
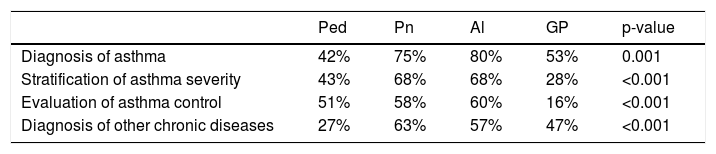
The conditions in which spirometry is used by physicians are depicted in Table 1.
Almost all agreed/totally agreed that spirometry results influence treatment decisions [94%Ped, 90%Pn, 100%AI, 81%GP (p=0.003)].
The majority of Ped, AI and GP (>85%) were interested in further training compared to 68% of Pn (p<0.001).
DiscussionGP/Ped report less familiarity on how to interpret and perform spirometry in asthmatic children, and less knowledge of ATS/ERS guidelines, than AI/Pn. However, almost all agreed that spirometric results influence their management decisions.
A multilevel approach is needed to change practices including identifying knowledge barriers and limitations in access across different settings and specialties, raising awareness and training.2,6 This study has several limitations, including the small sample size (<10% of members of each society) and likely bias due to preferences and increased interest of respondents. However, significant differences between the four specialities were identified. Acknowledgment of these gaps by the responsible authorities will facilitate the implementation of specific strategies adjusted to each specialty to improve the use of spirometry in the management of asthmatic children. Strategies should be considered across medical curricula and health directories on spirometry use. These are urgently needed to fulfil the goals of the National Program on Respiratory Diseases on this topic.
Conflicts of interestThe authors have no conflicts of interest to declare.