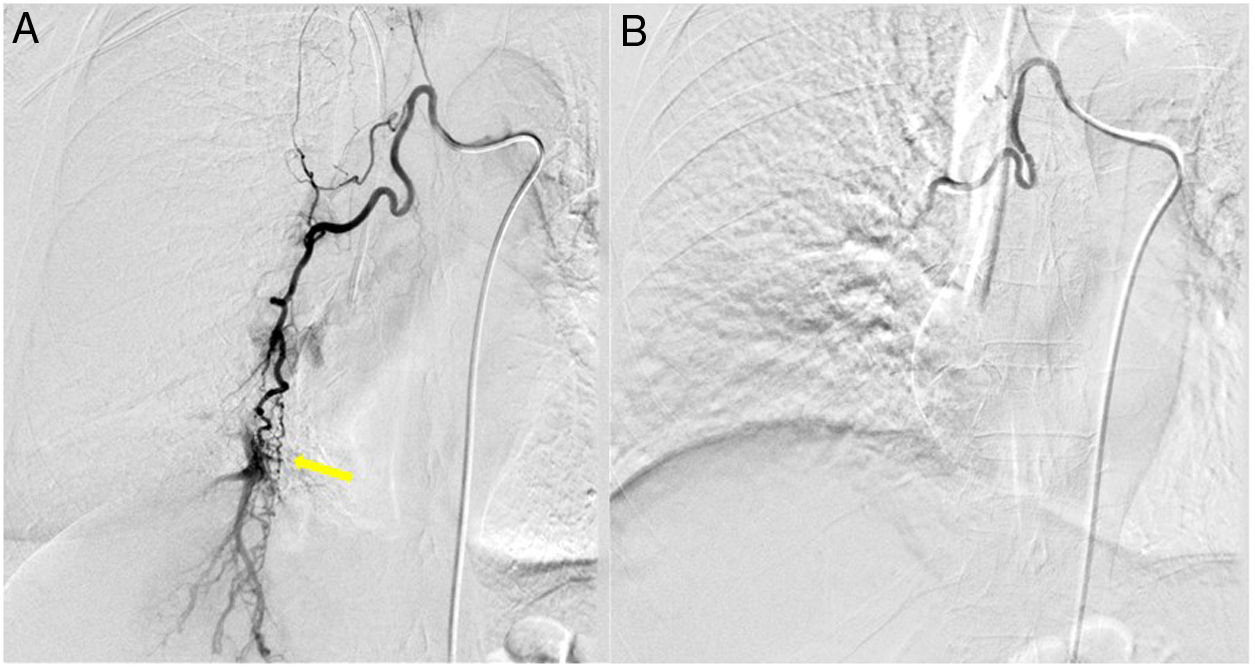
A 58-year-old woman, a butcher from her youth and a history of hemoptysis related to respiratory infection at the age of 30, was admitted into Intensive Care Unit for life-threatening hemoptysis and respiratory hypoxemic insufficiency. The bronchoscopy identified bleeding coming from the lower right lobe with an incipient clot. Computerized thoracic tomography revealed ground glass opacities in the middle and lower right lobes, probably indicative of blood filling alveoli. She was extubated 24h later and continued on antittussive treatment and amoxicillin/clavulanic acid until hemoptysis diminished in the following days. It was assumed that the risk of life-threatening rebleeding was high, so bronchial arterial embolization was performed. The arteriography detected the presence of a fistula connecting right bronchial (Fig. 1A) and pulmonary arteries and it was occluded with bead-block particles of 500–600μm. The subsequent control demonstrated flow extinction, the fistula was completely blocked (Fig. 1B). A week later, in the absence of hemoptysis, the patient was discharged.
Arterial malformations are commonly found in angiography conducted in hemoptysis.1 Cases of systemic-pulmonary circulation shunts have been reported within parenchymal lung involvement, mostly due to bronchiectasis2 or tuberculosis sequelaes,3 and rarely due to hereditary haemorragic telangiectasia.4 We present an elderly woman with a congenital brochial-pulmonary artery fistula and life-threatening hemoptysis, who was embolized with inmediate successful angiographic result. Embolization is seen as a safe and effective treatment for life-threatening hemoptysis, recurrence rates depend on different ethiologies.1 Our patient has a considerable risk of rebleeding, that may lead to repeat embolization or elective surgery in the future.
Conflicts of interestThe authors have no conflicts of interest to declare.
FundingThere is no funding for this manuscript.